the Creative Commons Attribution 4.0 License.
the Creative Commons Attribution 4.0 License.
Vertebral osteomyelitis and epidural abscess due to Listeria monocytogenes – case report and review of literature
Olayinka Ibironke Adebolu
Jennifer Sommer
Abiodun Benjamin Idowu
Nicole Lao
We describe a case of native vertebral osteomyelitis (NVO) secondary to Listeria monocytogenes in a patient with polymyalgia rheumatica receiving chronic steroids. Treatment required surgical debridement of the epidural phlegmon and combination therapy with intravenous ampicillin and gentamicin.
- Article
(1612 KB) - Full-text XML
- BibTeX
- EndNote
Listeria typically causes self-limited gastroenteritis; however, severe infections such as endovascular listeriosis and neurolisteriosis (brain abscess, rhombencephalitis) occur in high-risk patient subgroups such as pregnant women, immunocompromised patients, and those at extreme ages.
Listeria does not typically invade native joints; native vertebrae infection is even more rare. Bone and joint Listeria infections are primarily reported in those with prosthetic devices. We report a case of Listeria monocytogenes native vertebral osteomyelitis (NVO) and reviewed the published literature.
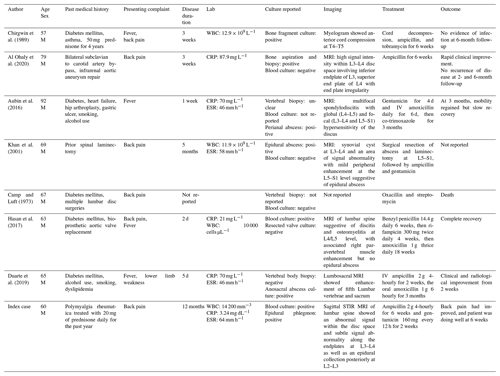
Embase, Google Scholar, and PubMed databases were comprehensively searched for the following terms: “listeria”, “listeria monocytogenes”, “arthritis”, “osteomyelitis”, “vertebrae osteomyelitis”, “spondylodiscitis”, and “discitis”. Reference lists of relevant articles were reviewed for potential studies. A total of nine cases have been documented: only seven reported in English language were examined in this study (Table 1). We excluded reports by Fernández de Orueta et al. (2011) and Schinagl et al. (2003) because they were in other languages.
A 60-year-old male grocery store worker from the Midwestern United States presented to the emergency room with acute exacerbation of lower back pain. He reported inability to get up on his feet and suffered multiple falls in the preceding months. The pain radiated down his right leg with associated right-thigh paresthesia. He denied fever but reported intermittent night sweats and new-onset loss of bowel control. His past medical history was significant for polymyalgia rheumatica treated with 20 mg of prednisone daily for the past year. A period of 6 months ago, he underwent endoscopy and colonoscopy in the context of chronic diarrhea. The stool study for enteric pathogens was negative. He had no personal history of diabetes, intravenous drug use, chronic cough, or weight loss. There was no history of travel outside the United States, and his HIV screen was negative.
On presentation, he was afebrile with a pulse rate of 101 beats min−1, blood pressure of mmHg, and respiratory rate of 16 breaths min−1. The lumbar spine was tender. Muscle strength was in bilateral lower extremities with normal sensation and intact anal sphincteric tone. His white blood cell (WBC) count was 14 200 mm−3, hemoglobin was 11.8 g dL−1, C-reactive protein (CRP) was 3.24 mg dL−1 (reference: <1.0 mg dL−1), the erythrocyte sedimentation rate (ESR) was 64 mm h−1 (reference: 0–20 mm h−1), creatinine was 3.24 mg dL−1, and the glomerular filtration rate (GFR) was 53 mL min−1 1.73 m−2. Two sets of blood cultures grew Listeria monocytogenes identified via matrix-assisted laser desorption/ionization time-of-flight mass spectrometry (MALD-TOF). The organism was susceptible to ampicillin (MIC 0.5) and penicillin (MIC 0.25). A transesophageal echocardiogram revealed no valvular abnormality.

Figure 1Sagittal STIR MR image of the lumbar spine showing an abnormal signal within the disc space and subtle signal abnormality along the endplates at L3–L4 as well as an epidural collection posteriorly at L2–L3 (originator: Jennifer Sommer).

Figure 2Sagittal T2 MR image of the lumbar spine again demonstrating an abnormal signal in the L3–L4 disc space and an epidural collection posteriorly at L2–L3 (originator: Jennifer Sommer).
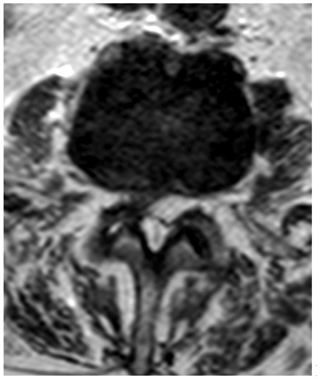
Figure 3Axial T2 MR image at the level of L2–L3 showing an epidural collection centred posteriorly and to the left with mass effect on the thecal sac (originator: Jennifer Sommer).
A lumbosacral spine X-ray showed moderate multi-level lumbar degenerative changes. Non-contrasted Magnetic Resonance Imaging (MRI) of the lumbar spine revealed an abnormal signal within the disc space and subtle signal abnormality along the endplates at L3–L4 (Figs. 1 and 2). Additionally, there was a fluid collection within the epidural space posteriorly and to the left of the midline at L2–L3, with a marked mass effect on the thecal sac and severe canal stenosis (Fig. 3). These findings were concerning for discitis-osteomyelitis at L3–L4, with an epidural abscess posteriorly at L2–L3.
He underwent irrigation and debridement, including levels L2, L3, and L4 laminectomy and decompression of the phlegmon. Medial facetectomy and foraminotomy of L2–L4 and lateral decompression of the L2, L3, and L4 nerve roots were also done. Epidural phlegmon drained intra-operatively grew Listeria monocytogenes. A histopathologic specimen collected intraoperatively showed fibro-fatty tissue with acute-on-chronic inflammation and areas of tissue necrosis consistent with abscess tissue.
He was gradually tapered down from prednisone and discontinued. A peripherally inserted central catheter (PICC) was placed for the administration of ampicillin (2 g every 4 h for 6 weeks) and gentamicin (160 mg every 12 h for 2 weeks) at a skilled nursing facility. At 6 weeks post-treatment, the back pain had improved, and the patient was rehabilitating well. However, contrasted MRI of the lumbar spine showed post-surgical changes with evidence of discitis and osteomyelitis at L3–L4. At 6 months, subsequent non-contrasted lumbar spine MRI noted significant improvement in the previously reported L3–L4 disc signal and T2 hyperintensity.
Listerial NVO is a rare manifestation because Listeria does not commonly affect the musculoskeletal system, except if the patient is immunocompromised or has in situ prosthetic material (Corrah et al., 2010). Established risk factors for L. monocytogenes include pregnancy, neonates and age above 65 years, hematologic malignancy, end-stage renal disease, recipients of organ transplants, HIV, alcoholism, and patients with auto-immune diseases on immunosuppression with steroids and TNF inhibitors (Del Pozo et al., 2013; Schett et al., 2005; Kubota et al., 2021). We hypothesized that use of chronic steroids and exposure to contaminated processed food predisposed our patient to this unusual infection. However, listeriosis can occur without identifiable risk factors (Al Ohaly et al., 2020; Aubin et al., 2016).
Our case suggests that listerial NVO has an insidious course of infection. The index patient had back pain for over a year; Khan et al. (2001) diagnosed their patient 5 months after the onset of intermittent backache. In a review of 43 cases of listerial bone and joint infections (BJIs), 73 % of infections were subacute or chronic in onset (Charlier et al., 2012). Additionally, in most documented cases (Table 1), compared to osteomyelitis secondary to S. aureus, inflammatory markers in L. monocytogenes NVO may be mildly elevated.
Blood cultures should always be obtained as many patients are placed on empiric anti-staphylococcal antibiotics, with a disc aspirate not always done (or it may be negative given receipt of prior antibiotics). The preferred imaging is an MRI of the vertebral column because of its high sensitivity (≥90 %) (Love et al., 2000). In four out of the seven reviewed cases (Table 1) and this index case (Figs. 1–3), contrasted MRI showed increased T2-weighted signal intensity of the affected disc space. An echocardiogram is warranted if there is concern for concomitant endovascular listeriosis as listerial endocarditis caries high mortality (Shoai-Tehrani et al., 2019).
Management of listerial NVO is based on clinical presentation. Surgical intervention may be warranted if there is a significant neurological deficit, cord compression, recurrence despite appropriate antimicrobial therapy, destruction of the vertebrae with instability, or large epidural abscess (Berbari et al., 2015). In patients where vertebrae is infected secondary to hematogenous seeding from an infected cardiac valve, antibiotics alone may suffice for the native valve, while replacement should be considered for an infected prosthetic valve (Kumaraswamy et al., 2018). Treatment includes intravenous ampicillin or penicillin combined with gentamicin to achieve a synergistic bactericidal effect. In those allergic to penicillin, trimethoprim/sulfamethoxazole is an alternative with comparable therapeutic efficacy (Temple and Nahata, 2000). Similar to listerial endocarditis and listerial brain abscess, the treatment duration for most Listeria BJIs is 4 to 6 weeks, though treatment duration to achieve a cure could be protracted in patients with delayed therapeutic response (Charlier et al., 2012). De-augmentation of immunosuppression is warranted in patients on immunosuppressive medication.
Listeria monocytogenes is a rare cause of NVO and typically has an insidious disease course. Receipt of chronic steroids or anti-TNF blockers is an important risk factor. Infection as a cause of back pain in an immunocompromised host must always be excluded.
The authors obtained written informed consent from the patient before submitting the publication. This is a single case report that does not require the approval of our institutional review board.
| WBC | White blood cell |
| CRP | C-reactive protein |
| GFR | Glomerular filtration rate |
| ESR | Erythrocyte sedimentation rate |
| MIC | Minimum inhibitory concentration |
No data sets were used in this article.
TR was responsible for conceptualization, patient care, and review, editing, and supervision of the paper. JS was responsible for patient care, radiological data and substantive revision of the manuscript. OIA, NL, and ABI were responsible for conceptualization, the writing of the original draft, review, and editing.
The contact author has declared that neither they nor their co-authors have any competing interests.
Publisher's note: Copernicus Publications remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This paper was edited by Marjan Wouthuyzen-Bakker and reviewed by two anonymous referees.
Al Ohaly, R., Ranganath N., Saffe, M. G., and Shroff, A.: Listeria Spondylodiscitis: an uncommon aetiology of a common condition; a case report, BMC Infect Dis., 20, 559–563, https://doi.org/10.1186/s12879-020-05286-y, 2020.
Aubin, G. G., Boutoille, D., Bourcier, R., Caillon, J., Lepelletier, D., Bémer, P., and Corvec, S.: Unusual Case of Spondylodiscitis due to Listeria monocytogenes, J. Bone Joint Infect., 1, 7–9, https://doi.org/10.7150/jbji.13863, 2016.
Berbari, E. F., Souha, S. K., Kowalski, T. J., Darouiche, R. O., Widmer, A. F., Schmitt, S. K., Hendershot, E. F., Holtom, P. D., Huddleston III, P. M., Petermann, G. W., and Osmon, D. R.: 2015 Infectious diseases Society of America (IDSA) Clinical Practice Guidelines for the Diagnosis and Treatment of Native Vertebral Osteomyelitis in Adults, Clin. Infect. Dis., 61, e26–46, https://doi.org/10.1093/cid/civ482, 2015.
Camp, C. and Luft, W. C.: Listeria monocytogenes osteomyelitis, Guthrie Bull., 43, 32–38, 1973.
Charlier, C., Leclercq, A., Cazenave ,B., Desplaces, N., Travier, L., and Cantinelli, T.: Listeria monocytogenes-associated joints and bone infections: A study of 43 consecutive cases, Clin. Infect. Dis., 54, 240–248, https://doi.org/10.1093/cid/cir803, 2012.
Chirgwin, K. and Gleich, S.: Listeria Monocytogenes Osteomyelitis, Arch. Intern. Med., 149, 931–932, https://doi.org/10.1001/archinte.1989.00390040127026, 1989.
Corrah, T. W., Enoch, D. A., Aliyu, S. H., and Lever, A. M.: Bacteremia and subsequent vertebral osteomyelitis: a retrospective review of 125 patients, Q. J. Med., 104, 201–207, https://doi.org/10.1093/qjmed/hcq178, 2010.
Del Pozo, J. L., de la Garza, R. G., de Rada P. D., Ornilla, E., and Yuste, J. R.: Listeria monocytogenes septic arthritis in a patient treated with mycophenolate mofetil for polyarteritis nodosa: a case report and review of the literature, Int. J. Infect. Dis., 17, e132–e133, https://doi.org/10.1016/j.ijid.2012.11.005, 2013.
Duarte, F., Pinto, S. M., Trigo, A. C., Guimaraes, F., Pereira, R., Neno, R., Correia de Abreu, R., and Neves, I.: A rare presentation of Listeria monocytogenes infection: perianal abscess associated with lumbal spine osteits, IDCases, 15, e00488, https://doi.org/10.1016/j.idcr.2019.e00488, 2019.
Fernández de Orueta, L., Esteban Fernández, J., Aichner, H. F., and Casillas Villamor, A.: Listeria monocytogenes osteomyelitis, Med. Clin. (Barc)., 139, e1, https://doi.org/10.1016/j.medcli.2011.10.009, 2011.
Hasan, T., Chik, W., Chen, S., and Kok, J.: Successful treatment of Listeria monocytogenes prosthetic valve endocarditis using rifampicin and benzylpenicillin in combination with valve replacement, JMM Case Rep., 4, e005085, https://doi.org/10.1099/jmmcr.0.005085, 2017.
Khan, K. M., Pao, W., and Kendler, J.: Epidural abscess and vertebral osteomyelitis caused by listeria monocytogenes: case report and literature review, Scand. J. Infect. Dis., 33, 714–716, https://doi.org/10.1080/00365540110027033, 2001.
Kubota, T., Mori, Y., Yamada, G., Cammack, I., Shinohara, T., Matsuzaka, S., and Hoshi, T.: Listeria monocytogenes ankle osteomyelitis in a patient with rheumatoid arthritis on Adalimumab: A Report and Literature Review of Listeria monocytogenes osteomyelitis, Intern. Med., 60, 3171–3176, https://doi.org/10.2169/internalmedicine.5633-20, 2021.
Kumaraswamy, M., Do, C., Sakoulas, G., Nonejuie, P., Tseng, G. W., King, H., Fierer, J., Pogliano, J., and Nizet, V.: Listeria monocytogenes endocarditis: case report, review of literature, and laboratory evaluation of potential novel antibiotic synergies, Int. J. Antimicrob. Agents., 51, 468–478, https://doi.org/10.1016/j.ijantimicag.2017.12.032, 2018.
Love, C., Patel, M., Lonner, B. S., Tomas, M. B., and Palestro, C. J.: Diagnosing spinal osteomyelitis: a comparison of bone and Ga-67 scintigraphy and magnetic resonance imaging, Clin. Nucl. Med., 25, 963–977, https://doi.org/10.1097/00003072-200012000-00002, 2000.
Schett, G., Herak, P., Graninger, W., Smolen, J. S., and Aringer, M.: Listeria-associated arthritis in a patient undergoing etanercept therapy: case report and review of the literature, J. Clin. Microbiol., 43, 2537–2541, https://doi.org/10.1128/JCM.43.5.2537-2541.2005, 2005.
Schinagl, D. A., Kappelle, A. C., van der Maazen, R. W., and Bussink, J.: The importance of a complete diagnostic workup in patients with non-traumatic (partial) paraplegia, Ned Tijdschr Geneeskd.,147 (52), 2565-9, 14723022, 2003.
Shoai-Tehrani, M., Pilmis, B., Maury, M. M., Robineau, O., Disson, O., Jouvion, G., Coulpier, G., Thouvenot, P., Bracq- Dieye, H., Vales, G., Leclercq, A., Lecuit, M., Charlier, C., and Listeria endovascular infections study group: Listeria monocytogenes-associated endovascular infections: A study of 71 consecutive cases, J. Infect., 79, 322–331, https://doi.org/10.1016/j.jinf.2019.07.013, 2019.
Temple, M. E. and Nahata, M. C.: Treatment of Listeriosis, Ann. Pharmacother., 34, 656–661, https://doi.org/10.1345/aph.19315, 2000.