Bialecki, J., Bucsi, L., Fernando, N., Foguet, P., Guo, S., Haddad, F.,
Hansen, E., Janvari, K., Jones, S., Keogh, P., Mchale, S., Molloy, R., Mont,
M. A., Morgan-Jones, R., Ohlmeier, M., Saldaña, A., Sodhi,
N., Toms, A., Walker, R., and Zahar, A.: Hip and Knee Section, Treatment, One
Stage Exchange: Proceedings of International Consensus on Orthopedic
Infections, J. Arthroplasty, 34, S421–S426, https://doi.org/10.1016/j.arth.2018.09.026, 2019.
Byren, I., Bejon, P., Atkins, B. L., Angus, B., Masters, S., McLardy-Smith,
P., Gundle, R., and Berendt, A.: One hundred and twelve infected
arthroplasties treated with “DAIR” (debridement, antibiotics and implant
retention): antibiotic duration and outcome, J. Antimicrob. Chemother.,
63, 1264–1271, 2009.
Chen, A. F., Heller, S., and Parvizi, J.: Prosthetic joint infections, Surg.
Clin., 94, 1265–1281, 2014.
Cooper, H. J. and Della Valle, C. J.: The two-stage standard in revision
total hip replacement, Bone Joint J., 95-B, 84–87, 2013.
Dale, H., Fenstad, A. M., Hallan, G., Havelin, L. I., Furnes, O., Overgaard,
S., Pedersen, A. B., Kärrholm, J., Garellick, G., and Pulkkinen, P.:
Increasing risk of prosthetic joint infection after total hip arthroplasty:
2,778 revisions due to infection after 432,168 primary THAs in the Nordic
Arthroplasty Register Association (NARA), Acta Orthop., 83, 449–458,
2012.
Deegan, B. F., Richard, R. D., Bowen, T. R., Perkins, R. M., Graham, J. H.,
and Foltzer, M. A.: Impact of chronic kidney disease stage on
lower-extremity arthroplasty, Orthopedics, 37, e613–e618,
https://doi.org/10.3928/01477447-20140626-51, 2014.
Ford, A. N., Holzmeister, A. M., Rees, H. W., and Belich, P. D.:
Characterization of outcomes of 2-stage exchange arthroplasty in the
treatment of prosthetic joint infections, J. Arthroplasty, 33,
S224–S227, 2018.
Furnes, O., Lie, S. A., Espehaug, B., Vollset, S. E., Engesaeter, L. B., and
Havelin, L. I.: Hip disease and the prognosis of total hip replacements: a
review of 53 698 primary total hip replacements reported to the Norwegian
arthroplasty register 1987–99, J. Bone Joint Surg. Br., 83, 579–586, https://doi.org/10.1302/0301-620X.83B4.11223, 2001.
Gomez, M. M., Tan, T. L., Manrique, J., Deirmengian, G. K., and Parvizi, J.:
The fate of spacers in the treatment of periprosthetic joint infection,
J. Bone Joint Surg., 97, 1495–1502, https://doi.org/10.2106/JBJS.N.00958, 2015.
Kandel, C. E., Jenkinson, R., Daneman, N., Backstein, D., Hansen, B. E.,
Muller, M. P., Katz, K. C., Widdifield, J., Bogoch, E., Ward, S., Sajja, A.,
Jeldes, F. G., and McGeer, A.: Predictors of Treatment Failure for Hip and
Knee Prosthetic Joint Infections in the Setting of 1- and 2-Stage Exchange
Arthroplasty: A Multicenter Retrospective Cohort, Open forum Infect. Dis.,
6, ofz452, https://doi.org/10.1093/ofid/ofz452, 2019.
Kheir, M. M., Tan, T. L., Gomez, M. M., Chen, A. F., and Parvizi, J.:
Patients With Failed Prior Two-Stage Exchange Have Poor Outcomes After
Further Surgical Intervention, J. Arthroplasty, 32, 1262–1265,
https://doi.org/10.1016/j.arth.2016.10.008, 2017.
Kurtz, S., Ong, K., Lau, E., Mowat, F., and Halpern, M.: Projections of
primary and revision hip and knee arthroplasty in the United States from
2005 to 2030, J. Bone Joint Surg., 89, 780–785, https://doi.org/10.2106/JBJS.F.00222, 2007.
Lindgren, J. V., Gordon, M., Wretenberg, P., Kärrholm, J., and Garellick,
G.: Validation of reoperations due to infection in the Swedish Hip
Arthroplasty Register, BMC Musculoskelet. Disord., 15, 384, https://doi.org/10.1186/1471-2474-15-384, 2014.
Lok-Chi Man, S., Chau, W.-W., Chung, K.-Y., and Ki Wai Ho, K.:
Hypoalbuminemia and obesity class II are reliable predictors of
peri-prosthetic joint infection in patient undergoing elective total knee
arthroplasty, Knee Surgery and Related Research, 32, 21, https://doi.org/10.1186/s43019-020-00040-9, 2020.
McPherson, E. J., Woodson, C., Holtom, P., Roidis, N., Shufelt, C., and
Patzakis, M.: Periprosthetic total hip infection: outcomes using a staging
system, Clin. Orthop. Relat. Res., 403, 8–15, 2002.
Older, J.: Charnley low-friction arthroplasty: a worldwide retrospective
review at 15 to 20 years, J. Arthroplasty, 17, 675–680, 2002.
Ong, K. L., Kurtz, S. M., Lau, E., Bozic, K. J., Berry, D. J., and Parvizi,
J.: Prosthetic joint infection risk after total hip arthroplasty in the
Medicare population, J. Arthroplasty, 24, 105–109, 2009.
Parvizi, J. and Gehrke, T.: Definition of periprosthetic joint infection, J.
Arthroplasty, 29, 1331, https://doi.org/10.1016/j.arth.2014.03.009, 2014.
Parvizi, J., Zmistowski, B., Berbari, E. F., Bauer, T. W., Springer, B. D.,
Della Valle, C. J., Garvin, K. L., Mont, M. A., Wongworawat, M. D., and
Zalavras, C. G.: New definition for periprosthetic joint infection: From the
workgroup of the musculoskeletal infection society, Clin. Orthop.
Relat. R., 469, 2992–2994, https://doi.org/10.1007/s11999-011-2102-9, 2011.
Wang, Q., Goswami, K., Kuo, F. C., Xu, C., Tan, T. L., and Parvizi, J.:
Two-Stage Exchange Arthroplasty for Periprosthetic Joint Infection: The Rate
and Reason for the Attrition After the First Stage, J. Arthroplasty, 34,
2749–2756, https://doi.org/10.1016/j.arth.2019.06.021, 2019.
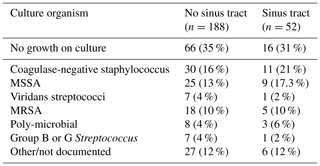
Xu, C., Wang, Q., Kuo, F.-C., Goswami, K., Tan, T. L., and Parvizi, J.: The
Presence of Sinus Tract Adversely Affects the Outcome of Treatment of
Periprosthetic Joint Infections, J. Arthroplasty, 34, 1227–1232.e2,
https://doi.org/10.1016/j.arth.2019.02.040, 2019.
Xu, C., Tan, T. L., Li, W. T., Goswami, K., and Parvizi, J.:
Complications-Infection Reporting Outcomes of Treatment for Periprosthetic
Joint Infection of the Knee and Hip Together With a Minimum 1-Year Follow-Up
is Reliable, J. Arthroplasty, 35, 1906–1911.e5,
https://doi.org/10.1016/j.arth.2020.02.017, 2020.
Zmistowski, B. and Alijanipour, P.: Risk factors for periprosthetic joint
infection, Periprosthetic Jt. Infect. Hip Knee, 15–40,
https://doi.org/10.1007/978-1-4614-7928-4_2, 2013.
Zmistowski, B., Karam, J. A., Durinka, J. B., Casper, D. S., and Parvizi, J.:
Periprosthetic joint infection increases the risk of one-year mortality,
J. Bone Joint Surg., 95, 2177–2184, https://doi.org/10.2106/JBJS.L.00789, 2013.