the Creative Commons Attribution 4.0 License.
the Creative Commons Attribution 4.0 License.
Corrigendum to “Assessment of risk factors for early-onset deep surgical site infection following primary total hip arthroplasty for osteoarthritis” published in J. Bone Joint Infect., 6, 443–450, 2021
Jonathan Bourget-Murray
Rohit Bansal
Alexandra Soroceanu
Sophie Piroozfar
Pam Railton
Kelly Johnston
Andrew Johnson
James Powell
- Article
(546 KB) - Full-text XML
- Original article
- BibTeX
- EndNote
The authors regret to report a mistake that has led to important errors in our original article (Bourget-Murray et al., 2021). The discrepancies in the results of the original article included Tables 2, 3, and 4. The correct methodology and results, including incidence, annual trend, perioperative outcomes, and risk factors of early-onset (≤90 d) deep surgical site infection (SSI) following primary THA for osteoarthritis in our study population, can be found below.
Deep SSIs were diagnosed by following the criteria outlined by the CDC/NHSN (CDC/NHSN, 2021). The ABJHI categorizes deep SSI by grouping patents who satisfy the CDC/NHSN definition of “deep surgical site infection” or “organ/space infection” together as both are a reflection of periprosthetic hip infections that extend deep to the fascia and involve the deep soft tissues and joint and therefore, from a surgical point of view, are treated in similar fashion.
There were 26 943 patients identified who received a primary THA for osteoarthritis between 1 January 2013 and 1 March 2020. Of these, 328 patients were diagnosed with a deep SSI within 90 d from surgery (Table 2). The cumulative incidence for early-onset deep SSI during the study period was 1.2 %. The annual rate of early-onset deep SSI was not found to have significantly decreased over the 7-year study period (p=0.29).
Table 2Annual number of confirmed complex surgical site infection cases within 90 d of surgery between January 2013 and March 2020.
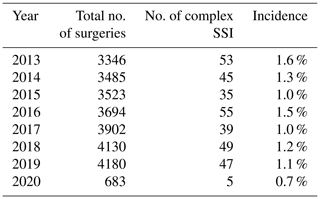
Total THA surgeries: 26 943; total deep SSI: 328. We used the Mann–Kendall trend test to detect monotonic trends in annual early-onset deep SSI rates during this timeframe.
Table 3Patient demographics and surgery characteristics.
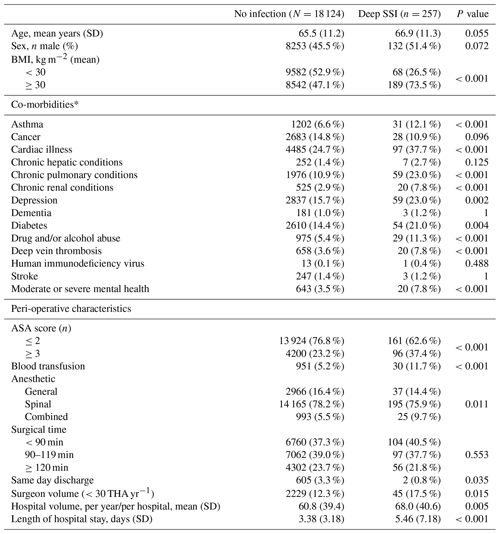
Fisher's exact test. * Co-morbidities were captured using health conditions classified in The CIHI Population Risk Grouper data: Cardiac conditions include acute myocardial infarction or arrest, arrhythmia, coronary artery disease, cardiac valve disease, malformation of cardiovascular system, heart failure. Chronic hepatic conditions include chronic liver disease including hepatic cirrhosis. Chronic pulmonary conditions include congenital disorder of the respiratory system, chronic obstructive pulmonary disease, pulmonary hypertension, respiratory failure, cystic fibrosis, tuberculosis disease and other chronic lung disease. Chronic renal conditions include chronic kidney disease/failure. Moderate or severe mental health includes delusional disorder (incl. schizophrenia), bipolar/manic mood disorder, eating disorder, intellectual disorder/delay and mental disorder resulting from brain injury or other illness. DVT, deep vein thrombosis; PE, pulmonary embolism.
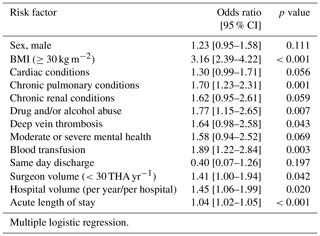
3.1 Risk factors for deep surgical site infection
Due to some missing patient demographic and surgery characteristic data, only 18 381 patients could be included for analysis, 257 of whom developed a deep SSI. Baseline patient and surgical characteristics investigated are summarized in Table 3. Multiple logistic regression analysis revealed BMI ≥30 kg m−2 (OR, 3.16 [95 % CI, 2.39 to 4.22]; p<0.001), chronic pulmonary disease (OR, 1.70 [95 % CI, 1.23 to 2.31]; p=0.001), drug and/or alcohol abuse (OR, 1.77 [95 % CI, 1.15 to 2.65]; p=0.007), deep vein thrombosis (OR, 1.64 [95 % CI, 0.98 to 2.58]; p=0.043), blood transfusion (OR, 1.89 [95 % CI, 1.22 to 2.84]; p=0.003), surgeon volume (<30 THA yr−1; OR, 1.41 [95 % CI, 1.00 to 1.94]; p=0.042), hospital volume (OR, 1.45 [p95 % CI, 1.06 to 1.99]; p=0.020), and acute hospital LOS (OR, 1.04 [95 % CI, 1.02 to 1.05]; p<0.001) were associated with increased risk of developing early-onset SSI following primary THA. The complete results from regression model are presented in Table 4.
3.2 Perioperative outcomes
Secondary outcomes were adjusted by age, sex, BMI (≥30 kg m−2), pre-surgery risk factor groups, anesthesia type, blood transfusion, same day discharged, acute LOS, surgeon volume, and hospital volume using multiple logistic regression. Developing a deep SSI within 90 d of surgery was associated with readmission within 90 d from surgery (OR, 19.43 [95 % CI, 14.76 to 25.54]; p<0.001) and associated with 90 d mortality (OR 7.24 [95 % CI, 2.45 to 17.21]; p<0.001).
This incidence of early-onset deep SSI is higher than we previously reported (Bourget-Murray et al., 2021). In addition, we report a significantly higher incidence of periprosthetic hip infection following THA for primary osteoarthritis compared to another recent Canadian publication from Ontario which showed a cumulative incidence of 0.48 % at 1 year and rising to 1.44 % at 15 years, but no estimate of early-onset deep SSIs (Arthroplasty Collaborative Mac™, 2020) However, both studies did not identify any change in annual rate of infection during the study period. Perhaps, our higher incidence is a reflection of the active surveillance across Alberta by IPC authorities which is performed until 90 d post-operatively (Canadian Institute for Health Information, 2020). This work establishes a reliable population-based baseline infection rate for early-onset deep SSI after THA for osteoarthritis.
Bourget-Murray, J., Bansal, R., Soroceanu, A., Piroozfar, S., Railton, P., Johnston, K., Johnson, A., and Powell, J.: Assessment of risk factors for early-onset deep surgical site infection following primary total hip arthroplasty for osteoarthritis, J. Bone Joint Infect., 6, 443–450, https://doi.org/10.5194/jbji-6-443-2021, 2021.
CDC/NHSN: Surveillance Definitions for Specific Types of Infections, Center for Disease Control National Healthcare Safety Network website, https://www.cdc.gov/nhsn/pdfs/pscmanual/9pscssicurrent.pdf, last access: 8 May 2021.
Arthroplasty Collaborative Mac™: Risk Factors for Periprosthetic Joint Infection Following Primary Total Hip Arthroplasty: A 15-Year, Population-Based Cohort Study, J. Bone Joint Surg. Am., 102, 503–509, 2020.
Canadian Institute for Health Information: Surgical Site Infections following Total Hip and Total Knee Replacement (SSIs) Provincial Surveillance. IPC Surveillance and Standards, Canadian Institute for Health Information website, https://www.albertahealthservices.ca/assets/healthinfo/ipc/hi-ipc-sr-hip-knee-ssi-protocol.pdf, last access: 3 May 2020.