the Creative Commons Attribution 4.0 License.
the Creative Commons Attribution 4.0 License.
Clinical practice variation in orthopedic infections: insights from the Musculoskeletal Infection Society (MSIS) and European Bone and Joint Infection Society (EBJIS) survey, 2023
Laura K. Certain
Irene K. Sigmund
In 2023, members of the Musculoskeletal Infection Society (MSIS) and the European Bone and Joint Infection Society (EBJIS) participated in a survey assessing their approaches to prevention, diagnosis, and management of orthopedic infections. The survey revealed notable differences between the two societies in several key areas, including requirements for smoking cessation prior to elective surgery, use of pre-operative skin and nasal antiseptics, application of local antibiotics in non-infected cases, preferred definitions of periprosthetic joint infection (PJI), use of alpha-defensin testing in pre-operative diagnosis, application of sonication of explanted implants, number of tissue samples obtained for microbiological and histological analysis, use of sequence-based diagnostics, and duration of antibiotic therapy. These findings demonstrate substantial variability in clinical practice among international experts in the field, highlighting the need for further research and consensus to harmonize strategies in orthopedic infection care.
- Article
(550 KB) - Full-text XML
- BibTeX
- EndNote
Orthopedic infections are among the most common infections encountered by infectious disease physicians. These conditions, including periprosthetic joint infection (PJI), fracture-related infection (FRI), vertebral osteomyelitis/diskitis (NVO), and diabetic foot infection, pose significant challenges to clinicians. Despite their prevalence, the optimal treatment approach remains debated, with cure rates influenced by both clinical and host-specific factors. Though in recent years we have gained some robust data on management (Li et al., 2019; Bernard et al., 2021; Obremskey et al., 2025), most treatment practices and guidelines are still largely based on expert opinion and retrospective studies.
Two professional societies promoting research and standards within this field are the European Bone and Joint Infection Society (EBJIS) and the Musculoskeletal Infection Society (MSIS, based in the United States). Members of these two societies are global leaders in the field of orthopedic infections, and many have clinical practices that focus almost exclusively on managing these challenging disease entities. While there is often general agreement among these experts on how best to manage a given infection, differences in daily clinical practice remain, likely due to ongoing gaps in the data available.
In 2023, we surveyed attendees of the MSIS annual meeting and members of EBJIS to gather data on current practices within this group of clinicians who focus on orthopedic infections. We present the results here, with the goal of highlighting areas of differing practice that point towards opportunities and needs for future research.
At the MSIS meeting in August 2023, meeting attendees were asked questions using Slido (http://slido.com, last access: 5 August 2023) during the meeting. There were 167 attendees at the meeting, of whom 60 were MSIS members. An email was sent out after the meeting to all MSIS members (N=246) to encourage additional responses and to ask additional questions. EBJIS conducted the survey via email only; an email inviting participation was sent to all EBJIS members (N=781) on 11 December 2023 and was closed on 2 June 2024. Standard summary statistics (means, percentages) were calculated as appropriate. Respondents who selected “I don't know” were excluded from the summary statistics for that question. A chi-squared test was used to determine whether differences between groups were statistically significant.
There were 128 respondents to the EBJIS survey (of whom 109 were EBJIS members, 85 %) and 86 respondents to the MSIS survey (53 members, 62 %). A majority of the EBJIS respondents were surgeons (97, 76 %), compared to a minority of the MSIS respondents (23, 27 %). In both groups, over 80 % of respondents were 30–60 years old, though the respondents to the EBJIS survey were further along in clinical practice (61 % in practice > 10 years compared to 43 % of the MSIS respondents). In both groups, about a third of respondents had more than half of their clinical practice devoted to management of orthopedic infection.
Table 3MSIS ID physician members responses to questions about the duration of antibiotic therapy in each clinical scenario.
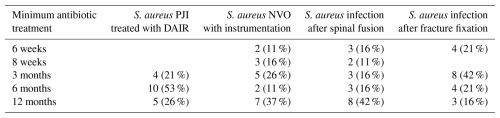
NVO = native vertebral osteomyelitis.
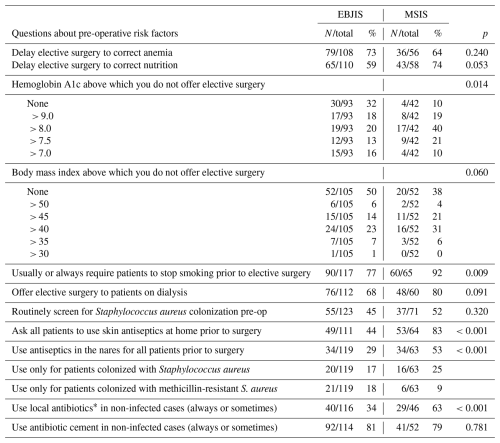
The first set of questions related to patient optimization before elective surgery (Table 1). There are a few notable differences between the two groups. For example, 92 % of MSIS respondents indicated that they required patients to quit smoking prior to elective surgery, compared to only 77 % of EBJIS respondents (χ2 (1, N=182) = 6.825, p=0.009). In addition, 83 % of MSIS respondents indicated asking all patients to use skin antiseptics at home prior to surgery, compared to only 44 % of EBJIS respondents (χ2 (1, N=175) = 24.96, p<0.001). MSIS respondents were also more likely to indicate the use of topical antibiotics (e.g., powders, calcium sulfate beads) in non-infected cases.
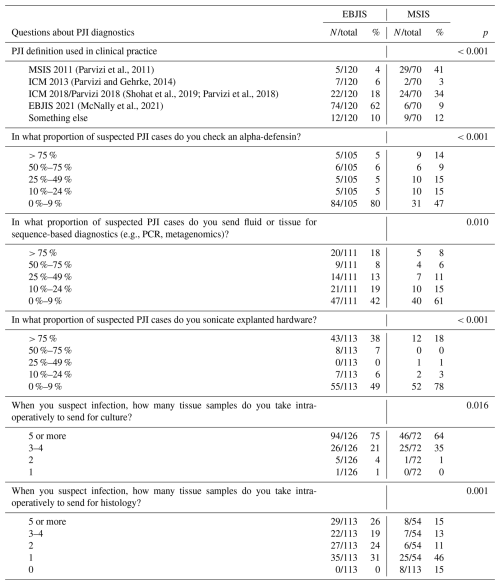
The next set of questions related to diagnosis of PJI (Table 2). Notably, there was little agreement within or between societies on the definition used in clinical practice, with approximately 10 % of respondents from each society using none of the standard PJI definitions. Alpha-defensin was used more frequently among the MSIS respondents, and sequence-based diagnostics were used more frequently by the EBJIS respondents. Use of sonication was bimodal in both groups, presumably due to variability in institutional capabilities. Members of EBJIS reported sending more samples for culture and histology.
There were 19 ID physician members of MSIS who responded to extended survey questions about the duration of antibiotic treatment in various clinical situations: Staphylococcus aureus PJI treated with debridement, antibiotics, and implant retention (DAIR); S. aureus native vertebral osteomyelitis (NVO) treated with instrumentation; S. aureus infection after spinal fusion; S. aureus infection after fracture fixation. There was very little agreement among this group of clinicians (Table 3). For example, for patients with S. aureus PJI managed with DAIR, 4 treated with systemic antibiotics for a minimum of 3 months, 10 for a minimum of 6 months, and 5 for a minimum of 12 months. Responses were similarly varied for spinal infections and for FRI. Of note, 16 of the 19 respondents reported treating > 100 musculoskeletal infections per year.
The survey results presented here provide perspective on current opinions and practices among clinicians specializing in the treatment of musculoskeletal infections. Discrepancies in clinical practice were observed in all areas queried: pre-operative risk management, PJI diagnosis, and treatment duration. These findings underscore substantial variation in clinical practice among experts and point to a clear need for further research to establish evidence-based consensus guidelines.
The responses about pre-operative risk assessment may reflect a difference in cultural approaches to risk management and infection prevention. The MSIS responses suggest a strategy favoring broader preventive measures, even if the absolute benefit is small or unknown; the EBJIS responses suggest more limited interventions. These contrasting philosophies are evident in practices regarding smoking cessation prior to surgery, nasal decolonization, pre-operative skin antisepsis, and the use of local antibiotics in non-infected cases. Such differences may reflect the influence of institutional culture and local interpretation of risk–benefit ratios in shaping clinical routines. The findings of this survey present an opportunity for both EBJIS and MSIS to reflect on the need for a more unified and transparent approach to infection prevention that incorporates both absolute and relative risk.
There was little consensus between and within societies on the definition of PJI used in clinical practice. This diversity is not surprising given the number of different published definitions and the lack of a universally accepted gold standard. Clinicians may default to the one they learned in training or the one most recently endorsed by their affiliated society. Fortunately, a new consensus definition is forthcoming, a result of collaborative effort between EBJIS, MSIS, the Infectious Disease Society of America (IDSA), the International Consensus Meeting (ICM), and the European Society of Clinical Microbiology and Infectious Diseases (ESCMID). The goal is to establish diagnostic criteria that improve accuracy and practicality in clinical practice and enhance comparability across clinical and research settings.
There are of course limitations to data gleaned by voluntary surveys. In addition, due to the make-up of the different societies and the fact that the MSIS survey was conducted in person at the meeting, the comparison is mainly between European surgeons and United States Infectious Disease physicians. The latter group may not be able to assess US surgical practices as accurately as their surgical colleagues. Many people attending the MSIS meeting and responding to the survey are not members of MSIS and may be non-clinicians or trainees who have not yet begun independent practice.
Despite these limitations, these data provide a snapshot of current practices in orthopedic infections across the US and Europe. Looking ahead, stronger collaboration between societies such as EBJIS and MSIS could play a vital role in advancing the field. Joint consensus initiatives, regular international conferences, and collaborative research efforts could help foster mutual understanding of regional practices and priorities. Furthermore, educational programs focusing on the interpretation and application of diagnostic tools may improve the consistency and accuracy of clinical decision-making. Comparative studies evaluating different treatment strategies, including the duration and route of antibiotic therapy, could also help establish clearer, evidence-based standards. Developing shared platforms for data collection and case registries may enhance global benchmarking and facilitate real-world evidence generation. Ultimately, a coordinated international effort can help reduce unwarranted variability in practice and support the development of more cohesive, patient-centered guidelines for the prevention and management of musculoskeletal infections.
Raw data are available from the authors upon request.
LC and IS collected the data. LC compiled and analyzed the data. IS and LC prepared the manuscript.
At least one of the (co-)authors is a member of the editorial board of the Journal of Bone and Joint Infection. The peer-review process was guided by an independent editor, and the authors also have no other competing interests to declare.
Participation in the surveys was voluntary, and no personally identifying data were collected.
Publisher’s note: Copernicus Publications remains neutral with regard to jurisdictional claims made in the text, published maps, institutional affiliations, or any other geographical representation in this paper. While Copernicus Publications makes every effort to include appropriate place names, the final responsibility lies with the authors. Views expressed in the text are those of the authors and do not necessarily reflect the views of the publisher.
The authors would like to acknowledge the executive boards and administrative support of each society for the years 2023–2025. The authors wrote this article on behalf of the MSIS and EBJIS executive boards. The board members of MSIS are Angela Hewlett, Brian Klatt, Alex McLaren, Andy Miller, Poorani Sekar, Thorsten Seyler, Aaron Tande, Ken Urish, and Marcy Wilkinson. The board members of EBJIS are Martin Clauss, Tristan Ferry, Annkathrin Mathe, Jan-Willem Metsemakers, Alex Soriano, Ricardo Sousa, and Marjan Wouthuyzen-Bakker.
This paper was edited by Willem-Jan Metsemakers and reviewed by two anonymous referees.
Bernard, L., Arvieux, C., Brunschweiler, B., Touchais, S., Ansart, S., Bru, J.-P., Oziol, E., Boeri, C., Gras, G., Druon, J., Rosset, P., Senneville, E., Bentayeb, H., Bouhour, D., Le Moal, G., Michon, J., Aumaître, H., Forestier, E., Laffosse, J.-M., Begué, T., Chirouze, C., Dauchy, F.-A., Devaud, E., Martha, B., Burgot, D., Boutoille, D., Stindel, E., Dinh, A., Bemer, P., Giraudeau, B., Issartel, B., and Caille, A.: Antibiotic Therapy for 6 or 12 Weeks for Prosthetic Joint Infection, N. Engl. J. Med., 384, 1991–2001, https://doi.org/10.1056/nejmoa2020198, 2021.
Li, H.-K., Rombach, I., Zambellas, R., Walker, A. S., McNally, M. A., Atkins, B. L., Lipsky, B. A., Hughes, H. C., Bose, D., Kümin, M., Scarborough, C., Matthews, P. C., Brent, A. J., Lomas, J., Gundle, R., Rogers, M., Taylor, A., Angus, B., Byren, I., Berendt, A. R., Warren, S., Fitzgerald, F. E., Mack, D. J. F. F., Hopkins, S., Folb, J., Reynolds, H. E., Moore, E., Marshall, J., Jenkins, N., Moran, C. E., Woodhouse, A. F., Stafford, S., Seaton, R. A., Vallance, C., Hemsley, C. J., Bisnauthsing, K., Sandoe, J. A. T. T., Aggarwal, I., Ellis, S. C., Bunn, D. J., Sutherland, R. K., Barlow, G., Cooper, C., Geue, C., Mcmeekin, N., Briggs, A. H., Sendi, P., Khatamzas, E., Wangrangsimakul, T., Wong, T. H. H. N., Barrett, L. K., Alvand, A., Old, C. F., Bostock, J., Paul, J., Cooke, G., Thwaites, G. E., Bejon, P., and Scarborough, M.: Oral versus Intravenous Antibiotics for Bone and Joint Infection, N. Engl. J. Med., 380, 425–436, https://doi.org/10.1056/NEJMoa1710926, 2019.
McNally, M., Sousa, R., Wouthuyzen-Bakker, M., Chen, A. F., Soriano, A., Vogely, H. C., Clauss, M., Higuera, C. A., and Trebše, R.: The EBJIS definition of periprosthetic joint infection, Bone Joint J., 103-B, 18–25, https://doi.org/10.1302/0301-620X.103B1.BJJ-2020-1381.R1, 2021.
Obremskey, W. T., O'Toole, R. V., Morshed, S., Tornetta, P., Murray, C. K., Jones, C. B., Scharfstein, D. O., Taylor, T. J., Carlini, A. R., DeSanto, J. M., Castillo, R. C., Bosse, M. J., Karunakar, M. A., Seymour, R. B., Sims, S. H., Weinrib, D. A., Churchill, C., Carroll, E. A., Pilson, H. T., Goodman, J. B., Holden, M. B., Miller, A. N., Sietsema, D. L., Stahel, P. F., Mir, H., Schmidt, A. H., Westberg, J. R., Mullis, B., Shively, K. D., Hymes, R. A., Konda, S. R., Vallier, H. A., Breslin, M. A., Smith, C. S., Crickard, C. V., Reid, J. S., Baker, M., Eglseder, W. A., LeBrun, C., Manson, T., Mascarenhas, D. C., Nascone, J., Pollak, A. N., Schloss, M. G., Sciadini, M. F., Degani, Y., Miclau, T., Weiss, D. B., Yarboro, S. R., McVey, E. D., Firoozabadi, R., Agel, J., Burgos, E. J., Gajari, V., Rodriguez-Buitrago, A., Tummuru, R. R., and Trochez, K. M.: Oral vs Intravenous Antibiotics for Fracture-Related Infections, JAMA Surg., 160, 276, https://doi.org/10.1001/jamasurg.2024.6439, 2025.
Parvizi, J. and Gehrke, T.: Definition of Periprosthetic Joint Infection, J. Arthroplasty, 29, 1331, https://doi.org/10.1016/j.arth.2014.03.009, 2014.
Parvizi, J., Zmistowski, B., Berbari, E. F., Bauer, T. W., Springer, B. D., Della Valle, C. J., Garvin, K. L., Mont, M. A., Wongworawat, M. D., and Zalavras, C. G.: New Definition for Periprosthetic Joint Infection: From the Workgroup of the Musculoskeletal Infection Society, Clin. Orthop. Relat. Res., 469, 2992–2994, https://doi.org/10.1007/s11999-011-2102-9, 2011.
Parvizi, J., Tan, T. L., Goswami, K., Higuera, C., Della Valle, C., Chen, A. F., and Shohat, N.: The 2018 Definition of Periprosthetic Hip and Knee Infection: An Evidence-Based and Validated Criteria, J. Arthroplasty, 33, 1309-1314.e2, https://doi.org/10.1016/j.arth.2018.02.078, 2018.
Shohat, N., Bauer, T., Buttaro, M., Budhiparama, N., Cashman, J., Della Valle, C. J., Drago, L., Gehrke, T., Marcelino Gomes, L. S., Goswami, K., Hailer, N. P., Han, S. B., Higuera, C. A., Inaba, Y., Jenny, J.-Y., Kjaersgaard-Andersen, P., Lee, M., Llinás, A., Malizos, K., Mont, M. A., Jones, R. M., Parvizi, J., Peel, T., Rivero-Boschert, S., Segreti, J., Soriano, A., Sousa, R., Spangehl, M., Tan, T. L., Tikhilov, R., Tuncay, I., Winkler, H., Witso, E., Wouthuyzen-Bakker, M., Young, S., Zhang, X., Zhou, Y., and Zimmerli, W.: Hip and Knee Section, What is the Definition of a Periprosthetic Joint Infection (PJI) of the Knee and the Hip? Can the Same Criteria be Used for Both Joints?: Proceedings of International Consensus on Orthopedic Infections, J. Arthroplasty, 34, S325–S327, https://doi.org/10.1016/j.arth.2018.09.045, 2019.