the Creative Commons Attribution 4.0 License.
the Creative Commons Attribution 4.0 License.
Costal osteomyelitis due to Bartonella henselae in a 10-year-old girl
Arnaud Salmon-Rousseau
Christelle Auvray
Quentin Besset
Claire Briandet
Claire Desplantes
Pascal Chavanet
Bartonella henselae is the bacterial agent responsible for cat scratch disease. This infection is frequently the cause of localized lymphadenitis in children. It is also sometimes responsible for endocarditis, encephalitis, hepatic peliosis and in rare cases osteomyelitis. We describe the second known case of unifocal thoracic osteomyelitis in a 10-year-old child.
- Article
(1381 KB) - Full-text XML
- BibTeX
- EndNote
Cat scratch disease is the most common zoonotic disease, affecting children and young adults in 80 % of cases (Mirouse et al., 2015). The first French cases were reported in 1950 by Robert Debré, who described the presence of spontaneously resolving adenopathies in the drainage area following cat scratches (Debre et al., 1950).
The so-called classic clinical form manifests itself as a single or single-site, unilateral, inflammatory, and sensitive lymphadenopathy. Atypical forms have been described with systemic expressions depending on the immune status of the host: examples include Parinaud's oculo-glandular syndrome, hepato-splenic abscess, endocarditis and encephalitis etc. (Leclainche and Bourrillon, 1996; Carithers, 1985). Bartonella osteoarticular infections are rare, and in fact the prevalence of these bone manifestations lies between 0.2 % and 0.3 % (Hajjaji et al., 2007; Maman et al., 2007) and affects mostly children; 75 % of cases are unifocal (Zellali et al., 2019), and the infection is usually localized in the spine (Zellali et al., 2019). The rib cage is rarely the site of such infections. There are a total of six cases of multifocal osteomyelitis with thoracic involvement and only one case of unifocal thoracic osteomyelitis in the literature.
Here, we report the second case of a child hospitalized for a suspected thoracic tumor that was finally found to be cat scratch disease, and we provide a review of the literature on osteoarticular B. henselae infections in the pediatric population.
We consulted the PubMed database to perform the present literature review.
We included systematic reviews, journals and case reports published in English since the first case was found in 1952.
We retained only cases reported for children, so all patients older than 18 years were excluded from the study.
The terms used in the search database were as follows: cat scratch disease, bone, bone infection, bone joint infection, bartonella, bartonellosis.
A 10-year-old girl presented with fever, diarrhea and diffuse muscle pain. Treatment with non-steroidal anti-inflammatory drugs and paracetamol was initiated by the treating physician, but the symptoms persisted and the patient developed bone pain in the sacroiliac, left thigh and left costal areas. She was hospitalized on the 10th day of clinical evolution, in a context of altered general condition and a weight loss equivalent to −3.5 % of total body weight. The clinical examination was unremarkable and did not reveal lymphadenopathy or hepato-splenomegaly. The first blood test showed white blood cells at 15.57 G/L, CRP of 150 mg/L and sterile blood cultures.
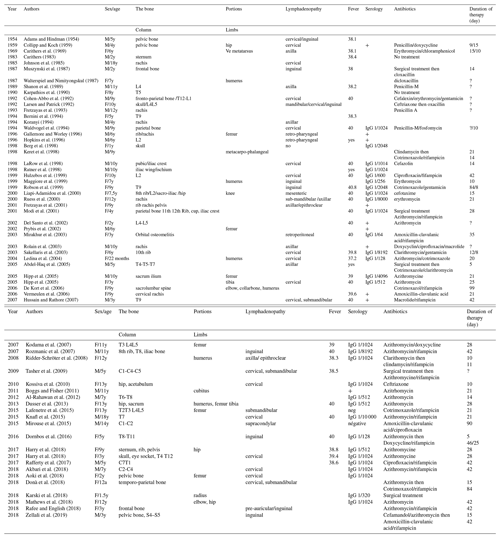
The thoracic–abdominal–pelvic CT scan showed moderate hepato-splenomegaly, a 20×23 mm left axillary ganglion (Fig. 1) and retro-pectoral lymph nodes larger than 1 cm. There were no abnormalities in the bone window.
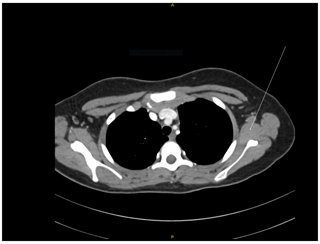
Figure 1Thoracic CT scan. The arrow shows the left axillary ganglion. Origin and source of radiology image: Department of Radiology CHU Dijon.
A technetium-99m bone scan revealed increased uptake in the left midrib.
Treatment with paracetamol and naproxen 10 mg/kg/d reduced the fever and allowed the patient to return home, and the diagnostic retained was then chronic aseptic osteomyelitis.
One month later, the child was again experiencing pain in the left costal area. Bioassay results showed hyperleukocytosis (10.7 G/L) and an elevated CRP level (37 mg/L). A new CT scan showed a single bone lesion on the anterior arch of the seventh left rib with a blown aspect and cortical lysis surrounded by a tissue sleeve. The lesion was 46 mm high, 64 mm deep and 34 mm wide, with a necrotic-looking tissue component (Fig. 2a).
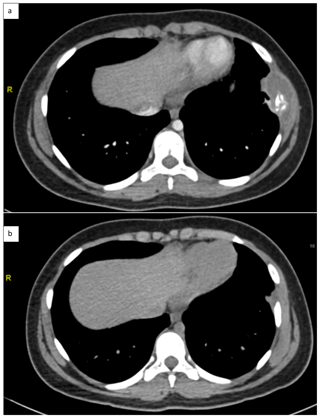
Figure 2Thoracic CT scan (a) at diagnosis (b) end of treatment. Origin and source of radiology images: Department of Radiology CHU Dijon.
The child was referred to the university hospital for a suspected chest tumor.
A surgical biopsy of the middle arch of the left seventh rib was performed, and the intraoperative findings revealed a purulent fluid with false membranes, revealing a lytic lesion of the rib.
Direct examination of pus after Gram staining found no bacteria. A few colonies of Staphylococcus lugdunensis were found after e days of culture. This result was considered as contamination of the sample taken by the surgeon.
Anatomo-pathological examination revealed granulomatous tissue, punctuated by small foci of necrosis surrounded by polymorphic inflammatory elements, rich in histiocytes and CD68+ macrophages around the foci. The periodic-acid–Schiff, Gram and Ziehl–Neelson stains were negative.
An interview with the girl's parents revealed the presence of kittens in the home. Further tests including Bartonella henselae serology returned with an IgG titre of 1/1280 (IFI technique), for a positivity threshold of 1/320. Bartonella henselae polymerase chain reaction (PCR) on whole blood was negative and 16S PCR on biopsy tissue was positive for Bartonella sp.
Treatment with a combination of azithromycin and rifampicin for 6 weeks completely improved the symptoms: lasting apyrexia, disappearance of pain in a few days and a weight gain of 3 kg at mid-treatment.
The anti-Bartonella IgG titre at the end of treatment was 1/640, and the chest CT scan revealed that the peri-costal collection had resolved and there was a favorable evolution of the bone lesion (Fig. 2b).
Follow-up at 6 months from the end of treatment found the girl in good general condition with no recurrence of fever or pain.
The diagnosis of osteoarticular infections in children is difficult. The incidence of all these infections is low, estimated to be between 7.1 and 22 per 100 000 population (Mitha et al., 2015; Grammatico-Guillon et al., 2013), and they can affect all parts of the skeleton even if they are predominately found in the lower limbs: 75 %–80 % of cases (Vial and Chiavassa-Gandois, 2012). The main bacteria that cause these infections are group B streptococcus in children under 3 months of age, Kingella kingae between 6 months and 4 years of age, and Staphylococcus aureus at all ages (Ferroni et al., 2013).
The main differential diagnosis for rapidly progressing bone disease is a neoplastic process (Massei et al., 2000).
Cat scratch disease affects an estimated 40 000 people worldwide, with 80 % of cases occurring in people under 18 years of age (Mirouse et al., 2015). The prevalence of osteomyelitis in Bartonella henselae varies between 0.2 % and 0.3 % (Hajjaji et al., 2007; Maman et al., 2007). Spinal injury is the most common manifestation (42 % of cases) and multifocal injury is seen in 25 % of cases (Zellali et al., 2019).
Our review of the literature identified 62 cases of B. henselae osteomyelitis in children published since 1954; only 7 cases included costal involvement (Table 1). The typical clinical picture is a child under 10 years of age with fever, cervical polyadenopathy and an average weight loss of 4.5 kg (Table 1). The scratch of a cat was observed in 20 out of 62 cases without necessarily being in the territory of the adenopathy (Table 1). Rare musculoskeletal manifestations (Maman et al., 2007) were reported for 30 out of 62 children, of which 20 % were arthralgia.
Biological examinations did not provide enough data to suggest a particular diagnosis: leukocytes were higher than 10 G/L for 21 out of 62 children. Non-discriminating inflammatory syndrome was generally found, with average CRP median of 20 mg/L (< 5–111 mg/mL).
Standard radiology was performed for 17 children, focusing on the painful segment. Osteolysis was sometimes found and in some cases associated with sclerosis or even a periosteal reaction within an infiltration of the surrounding soft tissues (Carithers, 1983; Johnson et al., 1985; Mazur-Melewska et al., 2015; Rohr et al., 2012). CT scans (performed on 25 children) confirmed bone destruction. MRI (31 children) was mostly used to evaluate the extent of lesions and whether they involved the bone marrow, adjacent tissues and the nervous system. Bone scintigraphy (23 children) offered the advantage of mapping the body, which revealed foci at a distance from the osteoarticular apparatus or detected abscesses on the liver and/or spleen in 15 out of 23 and 11 out of 23 children respectively. The potential of the PET scan has not yet been evaluated in this context.
Serology and molecular biology (polymerase chain reaction) techniques were used on tissue samples for microbiological diagnosis (Dusser et al., 2013; Hansmann et al., 2005). A total of 46 children were seropositive, and the anti-Bartonella IgG titre was greater than 1/512 for 26 of them. Only two children tested negative. Bartonella PCR was performed on 17 tissue samples and was positive on all samples; there were no false negatives in this series. The sensitivity of PCR analyses is estimated at 60 %–75 %, with high specificity allowing species diagnosis between Bartonella (Hansmann et al., 2005; Ratner et al., 1998; Eglantin et al., 2008).
Due to the rarity of osteoarticular forms of cat scratch disease, there are no defined antibiotic protocols. Macrolides were used for 52.0 % of children, 22 of whom received azithromycin. Beta-lactam antibiotics were also used in 34.8 % of children, fluoroquinolones in 7.6 % and doxycycline in 6 %.
When dual therapy was initiated (42.6 % of children), rifampicin was associated in 29.0 % and aminoglycosides in 13.6 %. Other combinations were either with Fosfomycin, chloramphenicol or cotrimoxazole.
In our case, the choice of antibiotic therapy (azithromycin and rifampicin) was motivated by their low minimal inhibitory concentrations reported in the literature (azithromycin 0.006–0.015 µg/mL, rifampicin 0.03–0.06 µg/mL), but also by their intracellular activity (Rolain et al., 2004; Bass et al., 1998).
The median duration of antibiotic therapy is 22 d (5–99 d).
Only 2 children (3.2 %) did not receive antibiotics, and 4 (6.4 %) laminectomy surgeries were performed.
Bartonella osteoarticular infections are rare in children, but should nonetheless be considered when a quickly progressing bone lesion is observed, a fortiori if there are signs of infection and there has been contact with animals, especially cats. Bartonella henselae serology should be carried out systematically in these cases, and close collaboration with the bacteriology laboratory should make it feasible to obtain a prompt diagnosis.
Consent was received from the patient prior to submission for publication.
No data sets were used in this article.
ASR, CD, PC, QB, CA and CB cared for the child, drafted the initial manuscript, and reviewed and revised the manuscript.
All authors approved the final paper as submitted and agree to be accountable for all aspects of the work.
The authors declare that they have no conflict of interest.
This paper was edited by Parham Sendi and reviewed by three anonymous referees.
Abdel-Haq, N., Abuhammour, W., Al-Tatari, H., and Asmar, B.: Disseminated cat scratch disease with vertebral osteomyelitis and epidural abscess, South Med. J., 98, 1142–1145, https://doi.org/10.1097/01.SMJ.0000163305.50078.63, 2005.
Adams, W. C. and Hindman, S. M.: Cat-scratch disease associated with an osteolytic lesion, J. Pediatr. Jun., 44, 665–669, https://doi.org/10.1016/s0022-3476(54)80007-2, 1954.
Akbari, S. H. A., Averill, C. E., Roland, J. L., Orscheln, R., and Strahle, J.: Bartonella henselae infection presenting as cervical spine osteomyelitis: case report, J. Neurosurg. Pediatr., 22, 189–194, https://doi.org/10.3171/2018.2.PEDS17600, 2018.
Al-Rahawan, M. M., Gray, B. M., Mitchell, C. S., and Smith, S. D.: Thoracic vertebral osteomyelitis with paraspinous mass and intraspinal extension: an atypical presentation of cat-scratch disease, Pediatr Radiol., 42, 116–119, https://doi.org/10.1007/s00247-011-2087-2, 2012.
Aoki Y, Kitazawa K, Sugawara D.: Femoral bone lesions accompanying cat-scratch disease. Arch Dis Child. 104(1):11. doi: 10.1136/archdischild-2018-314877. 2018
Bass, J. W., Freitas, B. C., Freitas, A. D., Sisler, C. L., Chan, D. S., Vincent, J. M., Person, D. A., Claybaugh, J. R., Wittler, R. R., Weisse, M. E., Regnery, R. L., and Slater, L. N.: Prospective randomized double blind placebo-controlled evaluation of azithromycin for treatment of cat-scratch disease, Pediatr. Infect. Dis. J., 17, 447–452, https://doi.org/10.1097/00006454-199806000-00002, 1998.
Berg, L. C., Norelle, A., Morgan, W. A., and Washa, D. M.: Cat-scratch disease simulating Histiocytosis X, Hum. Pathol., 29, 649–651, https://doi.org/10.1016/s0046-8177(98)80017-8, 1998.
Bernini, P. M., Gorczyca, J. T., and Modlin, J. F.: Cat-scratch disease presenting as a paravertebral abscess. A case report, J. Bone Joint Surg. Am., 76, 1858–1863, https://doi.org/10.2106/00004623-199412000-00014, 1994.
Boggs, S. R. and Fisher, G. R.: Bone pain and fever in an adolescent and his sibling. Cat scratch disease (CSD), Pediatr. Infect. Dis. J., 30, 93–94, https://doi.org/10.1097/inf.0b013e3181ebeade, 2011.
Carithers, H. A.: Cat-scratch disease associated with an osteolytic lesion, Am. J. Dis. Child, 137, 968–970, https://doi.org/10.1001/archpedi.1983.02140360032011, 1983.
Carithers, H. A.: Cat-scratch disease. An overview based on a study of 1,200 patients, Am. J. Dis. Child, 139, 1124–1133, https://doi.org/10.1001/archpedi.1985.02140130062031, 1985.
Carithers, H. A., Carithers, C. M., and Edwards Jr., R. O.: Cat scratch disease: the larger view, Pediatrics, 43, 629–631, 1969.
Cohen-Abbo, A., Cheatham, S., and Edwards, K.: Disseminated cat-scratch disease simulating neuroblastoma, Pediatr. Infect. Dis. J., 11, 1058–1060, 1992.
Collipp, P. J. and Koch, R.: Cat-scratch fever associated with an osteolytic lesion, N. Engl. J. Med., 260, 278–280, https://doi.org/10.1056/NEJM195902052600606, 1959.
Debre, R., Lamy, M., Jammet, M. L., Costil, L., and Mozziconacci, P.: ,Cat scratch disease, Sem. Hop., 30, 1895–1904, 1950.
De Kort, J. G. J. L., Robben, S. G. F., Schrander, J. J. P., and Van Rhijn, L. W.: Multifocal osteomyelitis in a child: a rare manifestation of cat scratch disease: a case report and systematic review of the literature, J. Pediatr. Orthop. B, 15, 285–288, https://doi.org/10.1097/01202412-200607000-00010, 2006.
Del Santo, M., Malorgio, C., Not, T., Maranzana, G., Cerasoli, G., Facchini, S., Zennaro, F., and Ventura, A.: Vertebral osteomyelitis in 2 children, Clin. Pediatr. (Phila), 41, 711–713, https://doi.org/10.1177/000992280204100911, 2002.
Donà, D., Nai Fovino, L., Mozzo, E., Cabrelle, G., Bordin, G., Lundin, R., Giaquinto, C., Zangardi, T., and Rampon, O.: Osteomyelitis in Cat-Scratch Disease: A Never-Ending Dilemma-A Case Report and Literature Review, Case Rep. Pediatr., 2018, 1679306, https://doi.org/10.1155/2018/1679306, 2018.
Dornbos, D., Morin, J., Watson, J. R., and Pindrik, J.: Thoracic osteomyelitis and epidural abscess formation due to cat scratch disease: case report, J. Neurosurg. Pediatr., 25, 713–716, https://doi.org/10.3171/2016.7.PEDS1677, 2016.
Dusser, P., Eyssette-Guerreau, S., and Koné-Paut, I.: Osteomyelitis in cat scratch disease: a case report and literature review, Arch. Pediatr., 20, 624–628, https://doi.org/10.1016/j.arcped.2013.03.013, 2013.
Eglantin, F., Hamdad, F., El Samad, Y., Monge, A. S., Sevestre, H., Eb, F., and Schmit, J. L.: The diagnosis of cat-scratch-disease-associated adenitis: diagnostic value of serology and polymerase chain reaction, Pathol. Biol., 56, 461–466, https://doi.org/10.1016/j.patbio.2008.07.020, 2008.
Ferroni, A., Al Khoury, H., Dana, C., Quesne, G., Berche, P., Glorion, C., snf Péjin, Z.: Prospective survey of acute osteoarticular infections in a French paediatric orthopedic surgery unit, Clin. Microbiol. Infect., 19, 822–828, https://doi.org/10.1111/clm.12031, 2013.
Fretzayas, A., Tapratzi, P., Kavazarakis, E., and Sinaniotis, C.: Multiorgan involvement in systemic cat-scratch disease, Scand. J. Infect. Dis., 25, 145–148, 1993.
Fretzayas, A., Papadopoulos, N. G., Moustaki, M., Bossios, A., Koukoutsakis, P., and Karpathios, T.: Unsuspected extralymphocutaneous dissemination in febrile cat scratch disease, Scand. J. Infect. Dis., 33, 599–603, https://doi.org/10.1080/00365540110026791, 2001.
Gallemore, G. and Worley, K.: Cat scratch disease presenting as multifocal osteitis, Tenn. Med., 89, 289e90, 1996.
Grammatico-Guillon, L., Maakaroun Vermesse, Z., Baron, S., Gettner, S., Rusch, E., and Bernard, L.: Paediatric bone and joint infections are more common in boys and toddlers: a national epidemiology study, Acta Paediatr., 102, e120–125, https://doi.org/10.1111/apa.12115, 2013.
Hajjaji, N., Hocqueloux, L., Kerdraon, R., and Bret, L.: Bone infection in cat-scratch disease: a review of the literature, J. Infect., 54, 417421, https://doi.org/10.1016/j.jinf.2006.10.045, 2007.
Hansmann, Y., DeMartino, S., Piémont, Y., Meyer, N., Mariet, P., Heller, R., Christmann, D., and Jaulhac, B.: Diagnosis of cat scratch disease with detection of Bartonella henselae by PCR: a study of patients with lymph node enlargement, J. Clin. Microbiol., 43, 3800–3806, https://doi.org/10.1128/JCM.43.8.3800-3806.2005, 2005.
Harry, O., Schulert, G. S., Frenck, J., Shapiro, A. H., Woltmann, J. L., Smith, J. A., and Grom, A. A.: Cat-Scratch Disease, a Diagnostic Consideration for Chronic Recurrent Multifocal Osteomyelitis, J. Clin. Rheumatol., 24, 287–290, https://doi.org/10.1097/RHU.0000000000000653, 2018.
Hipp, S. J., O'Shields, A., Fordham, L. A., Blatt, J., Hamrick, H. J., and Henderson, F. W.: Multifocal bone marrow involvement in cat-scratch disease, Pediatr. Infect. Dis. J., 24, 4724, https://doi.org/10.1097/01.inf.0000160993.52059.3a, 2005.
Hopkins, K. L., Simoneaux, S. F., Patrick, L. E., Wyly, J. B., Dalton, M. J., and Snitzer, J. A.: Imaging manifestations of cat-scratch disease, AJR Am. J. Roentgenol., 166, 435–438, https://doi.org/10.2214/ajr.166.2.8553962, 1996.
Hulzebos, C. V., Koetse, H. A., Kimpen, J. L., and Wolfs, T. F.: Vertebral osteomyelitis associated with cat-scratch disease, Clin. Infect. Dis., 28, 1310–1312, https://doi.org/10.1086/514787, 1999.
Hussain, S. and Rathore, M. H.: Cat scratch disease with epidural extension while on antimicrobial treatment, Pediatr. Neurosurg., 43, 164–166, https://doi.org/10.1159/000098395, 2007.
Johnson, J. F., Lehman, R. M., Shiels, W. E., and Blaney, S. M.: Osteolysis in cat-scratch fever, Radiology, 156, 373–374, https://doi.org/10.1148/radiology.156.2.4011899, 1985.
Karpathios, T., Fretzayas, A., Kakavakis, C., Garoufi, A., Courtis, C., and Christol, D.: Cat-scratch disease associated with osteomyelitis, Arch. Fr. Pediatr., 47, 369–371, 1990.
Karski, J., Matuszewski, Ł., Okoński, M., Pietrzyk, D., Karska, K., and Zaluski, M.: Cat Scratch Disease in a 1.5-year-old girl-Case report, Ann. Agric. Environ. Med., 25, 345–348, https://doi.org/10.26444/aaem/89547 2018.
Keret, D., Giladi, M., Kletter, Y., and Wientroub, S.: Cat-scratch disease osteomyelitis from a dog scratch, J. Bone Joint Surg. Br., 80, 766–767, P 1998.
Knafl, D., Lötsch, F., Burgmann, H., Goliasch, G., Poeppl, W., Ramharter, M., Thalhammer, F., and Schuster, C.: Hepatosplenic Abscesses and Osteomyelitis of the Spine in an Immunocompetent Adult with Cat Scratch Disease, Case Rep. Infect. Dis., 2015, 317260, https://doi.org/10.1155/2015/317260, 2015.
Kodama, Y., Maeno, N., Nishi, J., Imuta, N., Oda, H., Tanaka, S., Kono, Y., and Kawano, Y.: Multifocal osteomyelitis due to Bartonella henselae in a child without focal pain, J. Infect. Chemother., 13, 350–352, https://doi.org/10.1007/s10156-007-0548-1, 2007.
Koranyi, K.: Fever, back pain and pleural effusion in a four-year-old boy, Pediatr. Infect. Dis. J., 13, 657–672, 1994.
Kossiva, L., Vakaki, M., Pasparakis, D., Kallergi, K., Karavanaki, K., and Garoufi, A.: Hip monoarthritis in a child with cat-scratch disease: Rare manifestation, Pediatr. Int., 52, 680–681, https://doi.org/10.1111/j.1442-200X.2010.03152.x, 2010.
Lafenetre, M., Herbigneaux, R. M., Michoud, M., Descours, G., and Debillon, T.: Osteomyelitis in cat scratch disease: A case report and literature review, Arch. Pediatr., 23, 188–191, https://doi.org/10.1016/j.arcped.2015.11.009, 2015.
LaRow, J. M., Wehbe, P., and Pascual, A. G.: Cat-scratch disease in a child with unique magnetic resonance imaging findings, Arch. Pediatr. Adolesc. Med., 152, 394–396, https://doi.org/10.1001/archpedi.152.4.394, 1998.
Larsen, C. E. and Patrick, L. E.: Abdominal (liver, spleen) and bone manifestations of cat scratch disease, Pediatr. Radiol., 22, 353–355, https://doi.org/10.1007/BF02016255, 1992.
Leclainche, L. and Bourrillon, A.: Cat scratch disease in immunocompetent children, Arch. Pediatr., 3, 378–382, https://doi.org/10.1016/0929-693x(96)84695-1, 1996.
Ledina, D., Rincić, J., Ivić, I., Marasović, D., and Ledina, D.: A child with Bartonella henselae osteomyelitis of the right humerus, Acta Dermatovenerol. Croat., 12, 92–95, 2004.
Liapi-Adamidou, G., Tsolia, M., Magiakou, A. M., Zeis, P. M., Theodoropoulos, V., and Karpathios, T.: Cat scratch disease in 2 siblings presenting as acute gastroenteritis, Scand. J. Infect. Dis., 32, 317–319, https://doi.org/10.1080/00365540050165992, 2000.
Maggiore, G., Massei, F., Bussani, R., and Ventura, A.: Bone pain after lymphadenitis. Bartonella henselae granulomatous osteitis, Eur. J. Pediatr., 158, 165–166, https://doi.org/10.1007/s004310051040, 1999.
Maman, E., Bickels, J., Ephros, M., Paran, D., Comaneshter, D., Metzkor-Cotter, E., Avidor, B., Varon-Graidy, M., Wientroub, S., and Giladi, M.: Musculoskeletal manifestations of cat scratch disease, Clin. Infect. Dis., 45, 1535–1540, https://doi.org/10.1086/523587, 2007.
Massei, F., Messina, F., Talini, I., Massimetti, M., Palla, G., Macchia, P., and Maggiore, G.: Widening of the clinical spectrum of Bartonella henselae infection as recognized through serodiagnostics, Eur. J. Pediatr., 159, 416–419, https://doi.org/10.1007/s004310051298, 2000.
Mathews, D. M., Vance, K. M., McMahon, P. M., Boston, C., and Bolton, M. T.: An Atypical Case of Bartonella henselae Osteomyelitis and Hepatic Disease, Case Rep. Pediatr., 2018, 2750275, https://doi.org/10.1155/2018/2750275, 2018.
Mazur-Melewska, K., Mania, A., Kemnitz, P., Figlerowicz, M., and Służewski, W.: Cat-scratch disease: a wide spectrum of clinical pictures, Postepy Dermatol. Alergol., 32, 216–220, https://doi.org/10.5114/pdia.2014.44014, 2015.
Mirakhur, B., Shah, S. S., Ratner, A. J., Goldstein, S. M., Bell, L. M., and Kim, J. O.: Cat scratch disease presenting as orbital abscess and osteomyelitis, J. Clin. Microbiol., 41, 3991–3993, https://doi.org/10.1128/jcm.41.8.3991-3993, 2003.
Mirouse, G., Journe, A., Casabianca, L., Moreau, P. E., Pannier, S., and Glorion, C.: Bartonella henselae osteoarthritis of the upper cervical spine in a 14-year-old boy, Orthop. Traumatol. Surg. Res., 101, 519–522, https://doi.org/10.1016/j.otsr.2015.02.007, 2015.
Mitha, A., Boutry, N., Nectoux, E., Petyt, C., Lagrée, M., Happiette, L., and Martinot, A.: Hospital Network for Evaluating the Management of Infectious Diseases in Children Community-acquired bone and joint infections in children: a 1-year prospective epidemiological study, Arch. Dis. Child, 100, 126–129, https://doi.org/10.1136/archdischild-2013-305860, 2015.
Modi, S. P., Eppes, S. C., and Klein, J. D.: Cat-scratch disease presenting as multifocal osteomyelitis with thoracic abscess, Pediatr. Infect. Dis. J., 20, 1006–1007, https://doi.org/10.1097/00006454-200110000-00019, 2001.
Muszynski, M. J., Eppes, S., and Riley Jr., H. D.: Granulomatous osteolytic lesion of the skull associated with cat-scratch disease, Pediatr. Infect. Dis. J., 6, 199–201, https://doi.org/10.1097/00006454-198702000-00011, 1987.
Prybis, G., Eady, L., and Kotchmar Jr., S.: Chronic osteomyelitis associated with cat-scratch disease, J. South Orthop. Assoc., 11, 119–123, 2002.
Rafee, Y. and English, B. K.: Skull osteomyelitis as a rare complication of cat scratch disease, Avicenna J. Med., 8, 157–159, https://doi.org/10.4103/ajm.AJM_81_18, 2018.
Rafferty, J. R., Janopaul-Naylor, E., and Riese, J.: Torticollis and Fever in a Young Boy: A Unique Presentation of Cat-Scratch Disease With Vertebral Osteomyelitis and Epidural Phlegmon, Pediatr. Emerg. Care, 33, e164–e166, https://doi.org/10.1097/PEC.0000000000001330, 2017.
Ratner, L. M., Kesack, A., McCauley, T. R., and Disler, D. G.: Disseminated Bartonella henselae (cat-scratch disease): appearance of multifocal osteomyelitis with MR imaging, AJR Am. J. Roentgenol., 171, 1164–1165, https://doi.org/10.2214/ajr.171.4.9763023, 1998.
Ridder-Schröter, R., Marx, A., Beer, M., Tappe, D., Kreth, H. W., and Girschick, H. J.: Abscess-forming lymphadenopathy and osteomyelitis in children with Bartonella henselae infection, J. Med. Microbiol., 57, 519–524, https://doi.org/10.1099/jmm.0.47438-0, 2008.
Robson, J. M., Harte, G. J., Osborne, D. R., and McCormack, J. G.: Cat-scratch disease with paravertebral mass and osteomyelitis, Clin. Infect. Dis., 28, 274–278, https://doi.org/10.1086/515102, 1999.
Rohr, A., Saettele, M. R., Patel, S. A., Lawrence, C. A., and Lowe, L. H.: Spectrum of radiological manifestations of paediatric cat-scratch disease, Pediatr. Radiol., 42, 1380–1384, https://doi.org/10.1007/s00247-012-2451-x, 2012.
Rolain, J. M., Chanet, V., Laurichesse, H., Lepidi, H., Beytout, J., and Raoult, D.: Cat scratch disease with lymphadenitis, vertebral osteomyelitis, and spleen abscesses, Ann. N. Y. Acad. Sci., 990, 397–403, https://doi.org/10.1111/j.1749-6632.2003.tb07399.x, 2003.
Rolain, J. M., Brouqui, P., Koehler, J. E., Maguina, C., Dolan, M. J., and Raoult, D.: Recommendations for treatment of human infections caused by Bartonella species, Antimicrob. Agents Chemother., 48, 1921–1933, https://doi.org/10.1128/AAC.48.6.1921-1933.2004, 2004.
Rozmanic, V., Banac, S., Miletic, D., Manestar, K., Kamber, S., and Paparic, S.: Role of magnetic resonance imaging and scintigraphy in the diagnosis and follow-up of osteomyelitis in cat-scratch disease, J. Paediatr. Child Health, 43, 568–570, https://doi.org/10.1111/j.1440-1754.2007.01141.x, 2007.
Ruess, M., Sander, A., Brandis, M., and Berner, R.: Portal vein and bone involvement in disseminated cat-scratch disease: report of 2 cases, Clin. Infect. Dis., 31, 818–821, https://doi.org/10.1086/314029, 2000.
Sakellaris, G., Kampitakis, E., Karamitopoulou, E., Scoulica, E., Psaroulaki, A., Mihailidou, E., and Charissis, G.: Cat scratch disease simulating a malignant process of the chest wall with coexistent osteomyelitis, Scand. J. Infect. Dis., 35, 433–435, https://doi.org/10.1080/00365540310012262, 2003.
Shanon, A. B., Marchessault, J. H., and McDonald, P.: Cat-scratch disease associated with a vertebral osteolytic lesion, Pediatr. Infect. Dis. J., 8, 51–52, https://doi.org/10.1097/00006454-198901000-00013, 1989.
Tasher, D., Armarnik, E., Mizrahi, A., Liat, B. S., Constantini, S., and Grisaru-Soen, G.: Cat scratch disease with cervical vertebral osteomyelitis and spinal epidural abscess, Pediatr. Infect. Dis. J., 28, 848–850, https://doi.org/10.1097/INF.0b013e3181a3242e, 2009.
Vermeulen, M. J., Rutten, G. J., Verhagen, I., Peeters, M. F., and van Dijken, P. J.: Transient paresis associated with cat-scratch disease: case report and literature review of vertebral osteomyelitis caused by Bartonella henselae, Pediatr. Infect. Dis. J., 25, 1177–1181, https://doi.org/10.1097/01.inf.0000246807.14916.d3, 2006.
Vial, J. and Chiavassa-Gandois, H.: Limb infections in children and adults, Diagn. Interv. Imaging, 93, 530–546, https://doi.org/10.1016/j.diii.2012.03.014, 2012.
Waldvogel, K., Regnery, R. L., Anderson, B. E., Caduff, R., Caduff, J., and Nadal, D.: Disseminated cat-scratch disease: detection of Rochalimaea henselae in affected tissue, Eur. J. Pediatr., 153, 23–27, 1994.
Walterspiel, J. N. and Nimityongskul, P.: Positive bone scan in cat-scratch disease, Pediatr. Infect. Dis. J., 6, 944–945, https://doi.org/10.1097/00006454-198710000-00021, 1987.
Zellali, K., Benard, E., Smokvina, E., Belgaid, A., Labbé, F., and Bertrand, V.: Multifocal pelvic osteomyelitis in a child associated with cat-scratch disease: a case report and review of the literature, Paediatr. Int. Child Health, 39, 290293, https://doi.org/10.1080/20469047.2018.1476304, 2019.