the Creative Commons Attribution 4.0 License.
the Creative Commons Attribution 4.0 License.
Mid-term to long-term outcome and risk factors for failure of 158 hips with two-stage revision for periprosthetic hip joint infection
Moatasem Abuelnour
Conor McNamee
Abdul Basit Rafi
Wolf Hohlbein
Peter Keogh
James Cashman
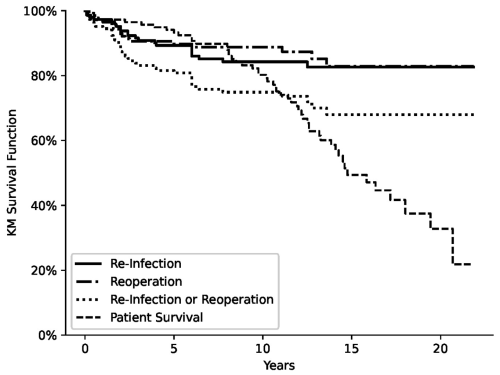
Introduction: This study aimed to evaluate infection-free survival and outcomes after two-stage revision surgery for hip periprosthetic joint infection (PJI) performed in a specialised arthroplasty unit over 20 years. Methods: We retrospectively identified 158 hips (154 patients) treated with two-stage revision surgery for hip PJI between 2001 and 2021. We analysed their data and presented their infection-free survival, re-operation rate, mortality, risk factors and complications. Results: The mean follow-up time was 9 (2 to 21.7) years. A total of 22 hips (13.9 %) were re-infected. The infection-free survival was 94.4 % at 2 years, 89.3 % at 5 years, 84.2 % at 10 years, and 82.6 % at 15 and 20 years. The re-operation rate for aseptic causes was 12 %, and the most common cause of re-operation was dislocation (7 %). The cumulative survival for re-operation for aseptic causes was 93.6 % at 2 years, 89.7 % at 5 years, 88.8 % at 10 years, and 82.8 % at 15 and 20 years. The cumulative survival for all-cause re-revision was 88.8 % at 2 years, 80.8 % at 5 years, 74.9 % at 10 years, and 68 % at 15 and 20 years. The mean Western Ontario and McMaster Universities Arthritis Index (WOMAC) hip score significantly improved from 68.3 at the pre-operative stage to 35.9 at 2.1 (2 to 3.3) years, 35.3 at 5.3 (5 to 8.4) years, 38.3 at 11.3 (10–15) years and 43.8 at 18.7 (16.5 to 21.7) years (p<0.01). Duration of antibiotics and gram-negative infection were the only predictive risk factors for re-infection. Conclusion: Our results of the two-stage revision protocol for hip PJI were satisfactory and comparable with the best reported outcomes.
- Article
(744 KB) - Full-text XML
- BibTeX
- EndNote
Periprosthetic joint infection (PJI) is uncommon (1 %–2 % after primary surgery and 3 %–4 % after revision) (Izakovicova et al., 2019 ) but represents a serious complication. The number of PJIs is increasing due to the rise in joint replacements worldwide, and this has a significant impact on economic and healthcare systems (Dobson and Reed, 2020). Despite the ongoing advances and interests in infection control, there is an increased cumulative revision rate due to infection after primary total hip replacement (THR) (Dale et al., 2012). Several consensus papers have been published for proper diagnosis and treatment of PJI (Parvizi et al., 2018), but still it remains controversial as to which patients might benefit from a single- versus two-stage procedure (Xu et al., 2020).
Nevertheless, the two-stage revision technique is still used by many surgeons since single-stage revision surgery is only recommended for specialised centres and in a group of patients with specific selection criteria (Klouche et al., 2012; Lum et al., 2020). Most of the published studies on two-stage revision have short-term to intermediate-term follow-up since longer follow-up of this group of elderly patients is usually not available due to multiple comorbidities, a high number of deaths and loss of follow-ups (Corona et al., 2020; Kildow et al., 2020).
This study aims to assess intermediate-term to long-term outcomes, the microbiological data and risk factors for failure of two-stage revision surgery for hip PJI in our arthroplasty unit over a period of 20 years. We report our survival outcomes, and we compare them with the published data of other arthroplasty units.
From 2001 to 2021, we retrospectively identified cases revised for hip PJI from our hospital records. We included patients with age ≥18 years, who had completed the two stages of hip PJI revision and whose data are available. We excluded patients who had single-stage revision, previous revision for PJI and multiple complex previous revisions for other causes and patients with tumour prostheses. Out of 14 002 primary THRs performed in our unit during this period, there were 1982 hips revised for all causes (14.2 %) and 191 revised for chronic PJI (1.4 %). A total of 158 hips (154 patients) revised for PJI met our inclusion criteria and were treated with the two-stage revision protocol. Most of our patients in this cohort presented with chronic infection (>4 weeks of symptoms) except seven cases, who had acute presentation (McPherson et al., 2002).
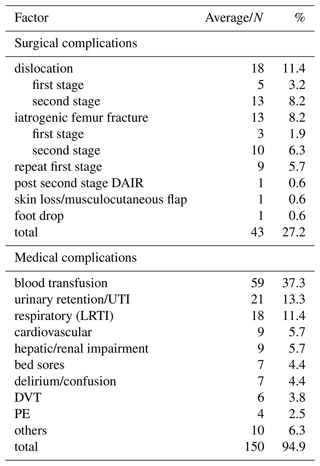
Demographic variables and comorbidities are described in Table 1. The main indication for primary surgery was osteoarthritis in 79.7 % of cases, and the average time from primary THR was 58.2 (1–273) months, while the average time between first and second stages of revision was 15 (2–84) weeks.
Diagnosis and definition of infection depended mainly on a range of clinical, laboratory and radiological tests. This was confirmed by intraoperative signs of PJI specially purulent fluids and implant loosening. No recognised diagnostic criteria were used, but more than one criterion was satisfied in all the cases. Surgical details of the two-stage procedure are described in Table 2. Patients were considered free of infection after the second stage if there was no growth on 5 d culture or only one positive culture with a low virulence or commensal microorganism, a return of serum C-reactive protein (CRP) to normal, and no clinical signs of infection. For the definition of successful clinical outcomes after revision of PJI, the Delphi-based international consensus has been adopted (Diaz-Ledezma et al., 2013). This includes (1) no clinical signs of infection, (2) no subsequent surgical intervention for infection and (3) no occurrence of PJI-related mortality.
Table 1Patients demographics (sample population n=158).
BMI, body mass index; ASA, American Society of Anesthesiologists; DM, diabetes mellitus; OA, osteoarthritis; RA, rheumatoid arthritis; AVN, avascular necrosis; THR, total hip replacement.
A total of 129 hips were available for ≥2 years follow-up. The mean follow-up time was 9 (2 to 21.7) years. The average time from second stage of revision surgery to reinfection was 36.1 (2–82) months. The follow-up regime in our unit included phone calls or clinic visits at 6 weeks, 6 months, 2 years, 5 years, 10 years and 15 years. The Western Ontario and McMaster Universities Arthritis Index (WOMAC) score (Bellamy et al., 1988) was collected at different follow-up points by our joint registry team and finally at the end of the study. We combined the follow-up years in intervals with means of 2.1 (2–5 years), 5.3 (5–10 years), 11.3 (10–15 years) and 18.7 (15–20 years). We contacted the patients or their relatives if there was no recent follow-up available on our record system. Patients could have non-routine clinic visit for clinical and radiological assessment of any worrisome signs.
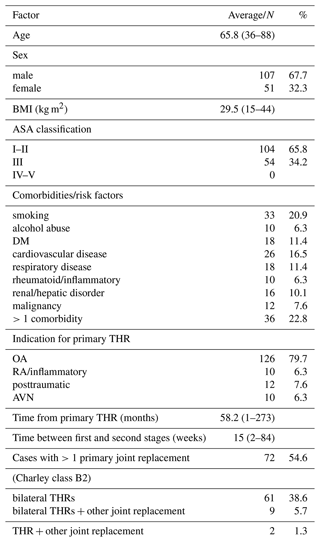
Table 2Operative details of the first and second stages (sample population n=158).
CUMARS: custom-made articulating spacer. ETO: extended trochanteric osteotomy.
Statistical analysis
Data were collected using a standardised electronic form. Continuous variables were summarised with mean and standard deviation and categorical variables with counts and percentages. The Kaplan–Meier estimator was used to calculate cumulative incidences of death, reinfection and reoperation. A multivariate cause-specific Cox proportional hazards regression model was fitted to reinfections. The results of this are reported as hazard ratios with 95 % confidence intervals. WOMAC scores were compared using the Kruskal–Wallis non-parametric test and Dunn's post hoc test to compare between time intervals. All statistical tests were two-sided, and significance was set at alpha = 0.05. Analyses were performed using Python 3.11 (Python Software Foundation) and Prism version 8 (GraphPad software).
A total of 147 hips completed the treatment, and 22 (13.9 %) hips were identified as re-infected or failed. The infection-free survival was 94.4 % at 2 years, 89.3 % at 5 years, 84.2 % at 10 years, and 82.6 % at 15 and 20 years (Fig. 1). In total, 11 hips did not proceed to the second stage (re-implantation). Analysis of these 11 hips has shown 5 hips did not have a second stage due to multiple comorbidities (ASA grade 3) and they died within an average of 10 (1–17) months, 3 hips did not have surgical data available for second stage, 2 hips had removal of spacer and Girdlestone resection due to severity of infection, and 1 hip had a dynamic spacer in (CUMARS technique, custom-made articulating spacer) (Tsung et al., 2014) and the patient was happy with outcome (WOMAC score 29) at their last follow-up (100 months). The two hips that ended with Girdlestone resection were considered failure and included in survival analysis.
There were 19 hips re-operated on for aseptic causes (12 %) (Table 3). The cumulative survival for re-operation for aseptic causes was 93.6 % at 2 years, 89.7 % at 5 years, 88.8 % at 10 years, and 82.8 % at 15 and 20 years (Fig. 1). Four hips of the re-operated cases had positive bacterial growth from intraoperative samples. In two hips the bacterial growth was considered significant as one hip developed severe infection after re-operation for a loose cup and ended with Girdlestone resection, and the other hip was kept on long-term antibiotics. Both hips were included in failure analysis. Taking the numbers of re-infected and re-operated cases together, the total number of all-cause re-revision is 41 hips (25.9 %). The cumulative survival for all-cause re-revision was 88.8 % at 2 years, 80.8 % at 5 years, 74.9 % at 10 years, and 68 % at 15 and 20 years (Fig. 1). There were three patients with significant radiological and clinical findings, but they were not re-operated on. One patient developed chronic dislocation 3 years after two-stage revision surgery. This patient continued to be treated conservatively due to poor compliance. Additionally, there were two patients with asymptomatic loosening of the femoral stem and acetabular cup respectively.
3.1 Functional outcome
At the preoperative stage the average WOMAC score was 68.3±16.2, and it improved significantly to 35.9±30.7 at the interval of 2.1 (2 to 3.3) years (p<0.001). Thereafter, the score remained relatively constant, 35.3 at 5.3 (5 to 8.4) years, 38.3 at 11.3 (10–15) years and 43.8 at 18.7 (16.5 to 21.7) years (p<0.01), maintaining the improvement from the preoperative stage but not showing further improvements.
Table 3Causes of re-operations other than recurrence of infection (sample population = 158).
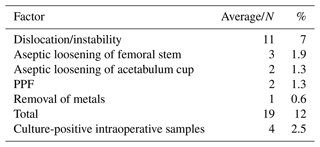
PPF: periprosthetic fracture.
3.2 Mortality
Mortality percentages increased progressively from 5.3 % at 2 years to 68.1 % at 20 years' follow-up after hip two-stage revision surgery. A total of 60 deaths (39 %) occurred by the time of the last follow-up. In the republic of Ireland, the overall mortality rate in 2022 in population aged ≥65 years is 3.8 % () (CSO, 2023). The mortality analysis included the 11 cases that did not proceed to the second stage; of these, 7 (63.6 %) were dead at the end of the study.
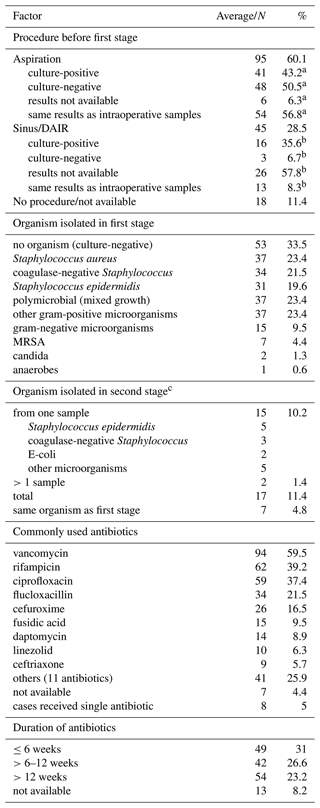
3.3 Microbiology
Results of microbiology are summarised in Table 4. There were 53 hips (33.5 %) that were culture-negative; the most common microorganism was Staphylococcus aureus (37 hips (23.4 %)) and then coagulase-negative Staphylococcus (34 hips (21.5 %)) and Staphylococcus epidermidis (31 hips (19.6 %)). Polymicrobial growth was recorded in 37 hips (23.4 %), and MRSA (methicillin-resistant Staphylococcus aureus) accounted for 7 hips (4.4 %). None of the culture-negative cases received antibiotics in the period of 2 weeks before the first stage or had autoimmune disease, previous revision for infection or any course of long-term suppressive antibiotics. Only four cases had sinus, and two cases had wash-outs before the first stage.
After the second stage, 17 hips (11.6 %) had culture-positive samples. Samples were considered insignificant if there was only one positive sample, it was a non-virulent microorganism and not the same microorganism isolated from first-stage intra-operative samples. Of these cases, 12 hips (8.2 %) were considered significant and had an extended antibiotic course for further 6–12 weeks. Follow-up and survival analysis of these 17 hips has shown that five hips (29.4 %) got re-infected.
3.4 Risk factors
The following risk factors had HR >1.5 but were not statistically significant (Table 5): alcoholism, avascular necrosis (AVN) as indication for primary THR, age >60 years, presence of sinus before first stage, re-implantation with uncemented and hybrid implants, gram-positive organisms (methicillin-sensitive, methicillin-resistant and coagulase-negative staphylococci), and isolation of microorganisms after the second stage. Of our cases, 54.6 % had >1 primary joint replacement (Charley class B2) (Dunbar et al., 2004), but it was not a predictor of worse outcome on the Cox regression analysis as we hypothesised. Samples infected with gram-negative microorganisms (hazard ratio, 24.3 (95 % CI, 2.82 to 208); p<0.01) and antibiotic duration >12 weeks (hazard ratio, 3.73 (95 % CI, 1.14 to 12.2); p=0.03) were the only predictors of re-infection.
Table 4Microbiology: microorganisms and antibiotics data (sample population n=158).
MRSA: methicillin-resistant Staphylococcus aureus. a Population sample n=95. b Population sample n=45. c Population sample n=147.
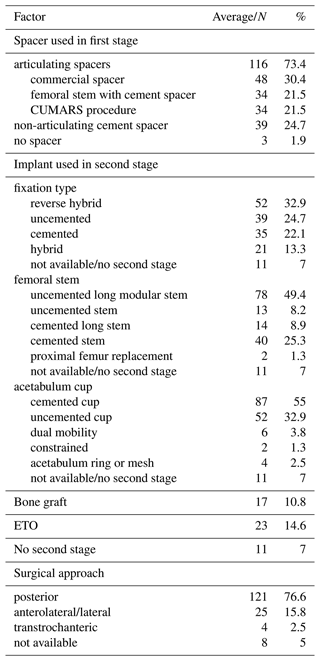
3.5 Complications
The most common surgical complications were dislocation (11.4 %), iatrogenic femur fracture (8.2 %) and repeated first stage (5.7 %) (Table 6). The average time from the second stage to dislocation was 16.7 (1–36) months. A total of 11 hips (7 %) were re-operated on for dislocation, and the rest was stable after closed reduction and non-surgical treatment. For the 13 hips with proximal femur fracture, 7 hips were managed surgically with cables, 3 hips were managed conservatively, and finally one hip was diagnosed 2 weeks later after the second stage and underwent internal fixation with plate and screws. Of the nine hips for which the first stage had been repeated, three hips did not proceed to the second stage due to early death, loss of follow-up and ongoing active infection that ended with Girdlestone hip resection. The other six hips successfully proceeded to second stage.
In this series of 158 hips revised with two stages protocol for PJI, survival without re-infection gradually declined until it plateaued, and 84.2 % patients were infection-free at 10 years and 82.6 % at ≥15 years' follow-up. Our results were comparable with best reported outcomes of similar treatment protocols (Petis et al., 2019; Biring et al., 2009; Kunutsor et al., 2015). Hips with previous non-revision interventions for infection like DAIR (debridement, antibiotics, and implant retention) or non-surgical treatment with antibiotics were included, and it did not seem they have worsened our survival outcomes. The reported success rate of two-stage revision is between 65 % to 95 % depending on the length of follow-up and authors' definition of failure (Kildow et al., 2020). Surgeons should be aware of the impact on patients' function, especially between the two stages of revision, increased morbidity and mortality, mental and psychological changes, and general frustration due to uncertainty and fear of recurrence of infection (Walter et al., 2024).
It is estimated that between 17 % and 30 % of patients do not proceed to the second stage during treatment for hip PJI (Gomez et al., 2015). In a series of 162 patients with PJI of hips and knees, Corona et al. (2020) reported an overall rate of eradication of infection of 71.6 %, but this rate increased to 80.6 % when they excluded patients who did not proceed to the second stage. They believed that this group of patients should be considered failure to avoid overestimating the success rate.
We preferred to describe the period without clinical signs of active infection after the second stage of revision as the “infection-free interval” rather than “eradication of infection” as surgeons usually look for serological and clinical signs of absence of active infection to end any invasive intervention; however, dormant infection cannot be excluded on this basis.
The overall mortality in this cohort is better than other studies (20 % at 10 years). Kildow et al. (2022) reported 40.1 % mortality at 5+ years' follow-up, and Wildeman et al. (2021) reported 45 % mortality rate at 10 years' follow-up. These high numbers of mortality may be attributed to the average age >65 years at time of revision and the impact of two-revision protocol on early- and mid-term mortalities.
The preoperative aspiration has shown less accuracy in PJI diagnosis. It is specific but less sensitive in excluding infection (Barker et al., 2021). The results of first-stage intra-operative samples has yielded 33.5 % negative cultures, which is within the range described in other studies (5 % to 42 %, Garabano et al., 2022). The outcome of culture-negative cases in PJI is controversial (Barker et al., 2021); however, only 4 out of 52 culture-negative cases (7.7 %) were documented as re-infection or failure in our cohort. New diagnostic modalities like next-generation sequencing and sonication have been described (Palan et al., 2019). However, surgeons should not expect worse outcomes if no organism is isolated, especially because other authors (Ibrahim et al., 2018; Li et al., 2023) have shown that culture-negative PJI cases have the same or better results compared to culture-positive ones.
Similar to our finding, Tsai et al. (2015) reported Staphylococcus aureus as the most common microorganism (29.9 %) in a series of 144 patients. Other studies reported coagulase-negative Staphylococcus as the most common microorganism (Petis et al., 2019; Biring et al., 2009). The isolation of Staphylococcus aureus was not associated with higher failure rates in our cohort as other studies have shown (Li et al., 2018). Also, polymicrobial infection (23.4 %) was common in our study but was not a risk factor for failure compared to other studies (Kildow et al., 2022). We could not identify any patient in our cohort on long-term suppressive antibiotics, and the current Delphi criteria (Diaz-Ledezma et al., 2013) do not consider patients on long-term suppressive antibiotics as failures.
Isolation of gram-negative microorganism and >12 week duration of antibiotics were predictors of re-infection in our cohort. Other studies described variable risk factors predictive of re-infection, for instance, young age (Bejon et al., 2010), morbid obesity (Houdek et al., 2015), use of chronic antibiotic suppression (Petis et al., 2019), methicillin-resistant staphylococci (Leung et al., 2011), gram-negative infection (Karczewski et al., 2023) and presence of a sinus tract (Xu et al., 2024). The lack of consensus on agreed risk factors is likely due to studies' heterogeneity and small numbers for statistical analysis.
The most common surgical complication was dislocation (8.2 %), which is similar to or less than other studies (Biring et al., 2009; McAlister et al., 2019). Other complications included iatrogenic femur fracture in 13 hips (8.2 %). Only two hips (1.3 %) were revised for postoperative periprosthetic femur fracture, which is significantly better than other similar reports (Petis et al., 2019). Surprisingly, only one case operated on by posterior approach had a foot drop due to sciatic nerve injury (0.6 %); this is similar to the risk of nerve injury after primary THR.
Other techniques have been developed like one-stage revision of PJI, with less complications, better function and similar outcomes (Goud et al., 2023). In a cost analysis study, Klouche et al. (2010) reported 70 % more cost with two-stage revision surgery. Nace et al. (2023) described a 1.5-stage revision in which a cement impregnated with 10 % antibiotics was used to fix the cemented components. No re-implantation is intended until aseptic failure of the first-stage implant. In our cohort, 21.5 % were treated similarly with the CUMARS procedure (Tsung et al., 2014); however all of them except one proceeded to second-stage revision in a short period.
Study limitations
This a single-centre retrospective study and inherently contains biases and lack of control or standardisation of different variables and comorbidities. Currently the most accepted and validated criteria for PJI diagnosis are the Musculoskeletal Infection Society (MSIS) criteria (Parvizi et al., 2018), but they were not applied to our retrospective cohort. The results of preoperative hip aspiration were only available in 60 % of our cases, and we did not have enough data for synovial cell counts. Our results could be overestimated due to the influence of different factors. The diagnosis was mainly based on surgeons' experience with clinical and serological confirmation; however, we can not exclude the possibility that non-infected hips have been revised with the two-stage protocol. The study retrospectively spanned >20 years, where different techniques, implants and antibiotic protocols have been introduced over this time. The average time between the two stages of revision was 15 weeks (2–84), which is longer than recommended. However, we are not aware of any study that has discussed the effect of time interval between the two stages of hip PJI revision on survival outcomes. Most cases that did not proceed to the second stage were not included in our analysis of failures. However, the number of cases without re-implantation was relatively small (11 cases (7 %)), compared to other studies that reported an average of 19 % of cases without re-implantation (Bourgonjen et al., 2021).
Our results for treatment of chronic hip PJI using two-stage revision protocol were similar to the best reported outcomes using the same protocol. Surgeons and patients should be aware of the complexity of hip PJI, the high mortality rate and controversy on what is successful for either the surgeon or the patient.
The data presented in this study are available upon request from the corresponding author. The data are not publicly available due to the privacy concerns regarding protected health information.
MA contacted the patients, collected and analysed the data, prepared the tables and figures, and wrote up the manuscript. CM did the statistics and the Cox regression model analysis. JC suggested and guided the project, prepared the ethics approval, and revised and corrected the final paper for publication. PK revised and corrected the final paper. Other authors contributed to data collection.
The contact author has declared that none of the authors has any competing interests.
The study was approved by the ethics committee in our hospital. Informed consent was not required, as this work was a retrospective review of patients' medical records, and no clinical photos were included.
Publisher's note: Copernicus Publications remains neutral with regard to jurisdictional claims made in the text, published maps, institutional affiliations, or any other geographical representation in this paper. While Copernicus Publications makes every effort to include appropriate place names, the final responsibility lies with the authors.
This paper was edited by Rihard Trebse and reviewed by two anonymous referees.
Barker, C. J., Marriot, A., Khan, M., Oswald, T., Tingle, S. J., Partington, P. F., Carluke, I., and Reed, M. R.: Hip aspiration culture: analysing data from a single operator series investigating periprosthetic joint infection, J. Bone Joint Infect., 6, 165–170, https://doi.org/10.5194/jbji-6-165-2021, 2021.
Bellamy, N., Buchanan, W. W., Goldsmith, C. H., Campbell, J., and Stitt, L. W.: Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee, J. Rheumatol., 15, 1833–1840, 1988.
Bejon, P., Berendt, A., Atkins, B. L., Green, N., Parry, H., Masters, S., McLardy-Smith, P., Gundle, R., and Byren, I.: Two-stage revision for prosthetic joint infection: predictors of outcome and the role of reimplantation microbiology, J. Antimicrob. Chemother., 65, 569–575, https://doi.org/10.1093/jac/dkp469, 2010.
Biring, G. S., Kostamo, T., Garbuz, D. S., Masri, B. A., and Duncan, C. P.: Two-stage revision arthroplasty of the hip for infection using an interim articulated Prostalac hip spacer: a 10- to 15-year follow-up study, J. Bone Joint Surgery, 91, 1431–1437, https://doi.org/10.1302/0301-620X.91B11.22026, 2009.
Bourgonjen, Y. P., Hooning van Duyvenbode, J. F. F., van Dijk, B., Nurmohamed, F. R. H. A., Veltman, E. S., Vogely, H. C., and van der Wal, B. C. H.: Long-term outcome of two-stage revision surgery after hip and knee prosthetic joint infections: an observational study, J. Bone Joint Infect., 6, 379–387, https://doi.org/10.5194/jbji-6-379-2021, 2021.
Central Statistics Office (CSO): Vital statistics yearly summary, Cork, Republic of Ireland, https://www.cso.ie/en/releasesandpublications/ep/p-vsys/vitalstatisticsyearlysummary2022 (last access: 10 October 2024), 2023.
Corona, P. S., Vicente, M., Carrera, L., Rodríguez-Pardo, D., and Corró, S.: Current actual success rate of the two-stage exchange arthroplasty strategy in chronic hip and knee periprosthetic joint infection, Bone Joint J., 102-B, 1682–1688, https://doi.org/10.1302/0301-620X.102B12.BJJ-2020-0792.R1, 2020.
Dale, H., Fenstad, A. M., Hallan, G., Havelin, L. I., Furnes, O., Overgaard, S., Pedersen, A. B., Kärrholm, J., Garellick, G., Pulkkinen, P., Eskelinen, A., Mäkelä, K., and Engesæter, L. B.: Increasing risk of prosthetic joint infection after total hip arthroplasty, Acta Orthop., 83, 449–458, https://doi.org/10.3109/17453674.2012.733918, 2012.
Diaz-Ledezma, C., Higuera, C. A., and Parvizi, J.: Success after treatment of periprosthetic joint infection: a Delphi-based international multidisciplinary consensus, Clin. Orthop. Rel. Res., 471, 2374–2382, https://doi.org/10.1007/s11999-013-2866-1, 2013.
Dobson, P. F. and Reed, M. R.: Prevention of infection in primary THA and TKA, EFORT open reviews, 5, 604–613, https://doi.org/10.1302/2058-5241.5.200004, 2020.
Dunbar, M. J., Robertsson, O., and Ryd, L.: What's all that noise? The effect of co-morbidity on health outcome questionnaire results after knee arthroplasty, Acta Orthopaedica Scandinavica, 75, 119–126, https://doi.org/10.1080/00016470412331294355, 2004.
Garabano, G., Gessara, A. M., Pesciallo, C. A., Martinez, J., and Del Sel, H.: Culture-negative Peri-prosthetic Joint Infection after Total Hip Arthroplasty Treatment Protocol and Outcomes in Acute and Chronic Cases, The archives of bone and joint surgery, 10, 806–811, https://doi.org/10.22038/ABJS.2022.51813.2559, 2022.
Gomez, M. M., Tan, T. L., Manrique, J., Deirmengian, G. K., and Parvizi, J.: The Fate of Spacers in the Treatment of Periprosthetic Joint Infection, J. Bone Joint Surg., 97, 1495–1502, https://doi.org/10.2106/JBJS.N.00958, 2015.
Goud, A. L., Harlianto, N. I., Ezzafzafi, S., Veltman, E. S., Bekkers, J. E. J., and van der Wal, B. C. H.: Reinfection rates after one- and two-stage revision surgery for hip and knee arthroplasty: a systematic review and meta-analysis, Arch. Orthop. Traum. Su., 143, 829–838, https://doi.org/10.1007/s00402-021-04190-7, 2023.
Houdek, M. T., Wagner, E. R., Watts, C. D., Osmon, D. R., Hanssen, A. D., Lewallen, D. G., and Mabry, T. M.: Morbid obesity: a significant risk factor for failure of two-stage revision total hip arthroplasty for infection, J. Bone Joint Surg., 97, 326–332, https://doi.org/10.2106/JBJS.N.00515, 2015.
Ibrahim, M. S., Twaij, H., and Haddad, F. S.: Two-stage revision for the culture-negative infected total hip arthroplasty : A comparative study, Bone Joint J., 100-B, 3–8, https://doi.org/10.1302/0301-620X.100B1.BJJ-2017-0626.R1, 2018.
Izakovicova, P., Borens, O., and Trampuz, A.: Periprosthetic joint infection: current concepts and outlook, EFORT open reviews, 4, 482–494, https://doi.org/10.1302/2058-5241.4.180092, 2019.
Karczewski, D., Scholz, J., Hipfl, C., Akgün, D., Gonzalez, M. R., and Hardt, S.: Gram negative periprosthetic hip infection: nearly 25 % same pathogen infection persistence at a mean of 2 years, Arch. Orthop. Traum. Su., 144, 5053–5059, https://doi.org/10.1007/s00402-023-05104-5, 2023.
Kildow, B. J., Della-Valle, C. J., and Springer, B. D.: Single vs 2-Stage Revision for the Treatment of Periprosthetic Joint Infection, J. Arthroplasty, 35, S24–S30, https://doi.org/10.1016/j.arth.2019.10.051, 2020.
Kildow, B. J., Springer, B. D., Brown, T. S., Lyden, E., Fehring, T. K., and Garvin, K. L.: Long Term Results of Two-Stage Revision for Chronic Periprosthetic Hip Infection: A Multicenter Study, J. Clin. Med., 11, 1657, https://doi.org/10.3390/jcm11061657, 2022.
Klouche, S., Sariali, E., and Mamoudy, P.: Total hip arthroplasty revision due to infection: a cost analysis approach, Orthop. Traumatol.-Sur., 96, 124–132, https://doi.org/10.1016/j.rcot.2010.02.005, 2010.
Klouche, S., Leonard, P., Zeller, V., Lhotellier, L., Graff, W., Leclerc, P., Mamoudy, P., and Sariali, E.: Infected total hip arthroplasty revision: one- or two-stage procedure?, Orthop. Traumatol.-Sur., 98, 144–150, https://doi.org/10.1016/j.otsr.2011.08.018, 2012.
Kunutsor, S. K., Whitehouse, M. R., Blom, A. W., Beswick, A. D., and INFORM Team: Re-Infection Outcomes following One- and Two-Stage Surgical Revision of Infected Hip Prosthesis: A Systematic Review and Meta-Analysis, PloS One, 10, e0139166, https://doi.org/10.1371/journal.pone.0139166, 2015.
Leung, F., Richards, C. J., Garbuz, D. S., Masri, B. A., and Duncan, C. P.: Two-stage total hip arthroplasty: how often does it control methicillin-resistant infection?, Clin. Orthop. Rel. Res., 469, 1009–1015, https://doi.org/10.1007/s11999-010-1725-6, 2011.
Li, F., Qiao, Y., Zhang, H., Cao, G., and Zhou, S.: Comparable clinical outcomes of culture-negative and culture-positive periprosthetic joint infections: a systematic review and meta-analysis, J. Orthop. Surg. Res., 18, 210, https://doi.org/10.1186/s13018-023-03692-x, 2023.
Li, Z. L., Hou, Y. F., Zhang, B. Q., Chen, Y. F., Wang, Q., Wang, K., Chen, Z. Y., Li, X. W., and Lin, J. H.: Identifying Common Pathogens in Periprosthetic Joint Infection and Testing Drug-resistance Rate for Different Antibiotics: A Prospective, Single Center Study in Beijing, Orthop. Surg,, 10, 235–240, https://doi.org/10.1111/os.12394, 2018.
Lum, Z. C., Holland, C. T., and Meehan, J. P.: Systematic review of single stage revision for prosthetic joint infection, World journal of orthopedics, 11, 559–572, https://doi.org/10.5312/wjo.v11.i12.559, 2020.
McAlister, I. P., Perry, K. I., Mara, K. C., Hanssen, A. D., Berry, D. J., and Abdel, M. P.: Two-Stage Revision of Total Hip Arthroplasty for Infection Is Associated with a High Rate of Dislocation, J. Bone Joint Surg., 101, 322–329, https://doi.org/10.2106/JBJS.18.00124, 2019.
McPherson, E. J., Woodson, C., Holtom, P., Roidis, N., Shufelt, C., and Patzakis, M.: Periprosthetic total hip infection: outcomes using a staging system, Clin. Orthop. Rel. Res., 403, 8–15, 2002.
Nace, J., Chen, Z., Bains, S. S., Kahan, M. E., Gilson, G. A., Mont, M. A., and Delanois, R. E.: 1.5-Stage Versus 2-Stage Exchange Total Hip Arthroplasty for Chronic Periprosthetic Joint Infections: A Comparison of Survivorships, Reinfections, and Patient-Reported Outcomes, J. Arthroplasty, 38, S235–S241, https://doi.org/10.1016/j.arth.2023.02.072, 2023.
Palan, J., Nolan, C., Sarantos, K., Westerman, R., King, R., and Foguet, P.: Culture-negative periprosthetic joint infections, EFORT open reviews, 4, 585–594, https://doi.org/10.1302/2058-5241.4.180067, 2019
Parvizi, J., Tan, T. L., Goswami, K., Higuera, C., Della Valle, C., Chen, A. F., and Shohat, N.: The 2018 Definition of Periprosthetic Hip and Knee Infection: An Evidence-Based and Validated Criteria, J. Arthroplasty, 33, 1309–1314.e2, https://doi.org/10.1016/j.arth.2018.02.078, 2018.
Petis, S. M., Abdel, M. P., Perry, K. I., Mabry, T. M., Hanssen, A. D., and Berry, D. J.: Long-Term Results of a 2-Stage Exchange Protocol for Periprosthetic Joint Infection Following Total Hip Arthroplasty in 164 Hips, J. Bone Joint Surg., 101, 74–84, https://doi.org/10.2106/JBJS.17.01103, 2019.
Tsai, J. C., Sheng, W. H., Lo, W. Y., Jiang, C. C., and Chang, S. C.: Clinical characteristics, microbiology, and outcomes of prosthetic joint infection in Taiwan, J. Microbiol. Immunol., 48, 198–204, https://doi.org/10.1016/j.jmii.2013.08.007, 2015.
Tsung, J. D., Rohrsheim, J. A., Whitehouse, S. L., Wilson, M. J., and Howell, J. R.: Management of periprosthetic joint infection after total hip arthroplasty using a custom made articulating spacer (CUMARS); the Exeter experience, J. Arthroplasty, 29, 1813–1818, https://doi.org/10.1016/j.arth.2014.04.013, 2014.
Walter, N., Mohokum, M., Loew, T., Rupp, M., and Alt, V.: Healing beyond the joint: Addressing mental health in periprosthetic joint infection in a prospective longitudinal study, J. Psychosomatic Res., 177, 111559, https://doi.org/10.1016/j.jpsychores.2023.111559, 2024.
Wildeman, P., Rolfson, O., Söderquist, B., Wretenberg, P., and Lindgren, V.: What Are the Long-term Outcomes of Mortality, Quality of Life, and Hip Function after Prosthetic Joint Infection of the Hip? A 10-year Follow-up from Sweden, Clin. Orthop. Rel. Res., 479, 2203–2213, https://doi.org/10.1097/CORR.0000000000001838, 2021.
Xu, C., Goswami, K., Li, W. T., Tan, T. L., Yayac, M., Wang, S. H., and Parvizi, J.: Is Treatment of Periprosthetic Joint Infection Improving Over Time?, J. Arthroplasty, 35, 1696–1702.e1, https://doi.org/10.1016/j.arth.2020.01.080, 2020.
Xu, H., Li, S., Liu, S., Li, S., Yin, Z., Du, Y., Weng, X., and Qian, W.: The presence of a sinus tract is associated with reinfection after two-stage revision surgery for prosthetic hip joint infection: a case-control study, BMC Musculoskel. Dis., 25, 721, https://doi.org/10.1186/s12891-024-07840-0, 2024.